The lecture of Death and Dying in the context of pandemics has had me reflecting on what death has looked like in various public health crises. The scene of Mark’s death in “The View From Here” was one of the first times I have seen a death from AIDS. I grew up after the worst of the HIV/AIDS crisis and often feel removed from that disease in many ways. Thinking about how at one point death from AIDS was inevitable, and something that could be planned to an extent, is so different from other infectious disease epidemics.
The first time I became aware of pandemic death was really during the Ebola outbreak between 2014-2016 in West Africa. I had been studying the psychology of death through courses and even research, but was so struck by how scary death looked in this setting. News reports showed images of individuals in full PPE carting away body bags, with weary onlookers keeping a distance. The last days were often painful for patients, likely dying of profuse hemorrhage, encephalopathy, or sudden death. If medical care wasn’t available early, death was likely and would often occur quickly.
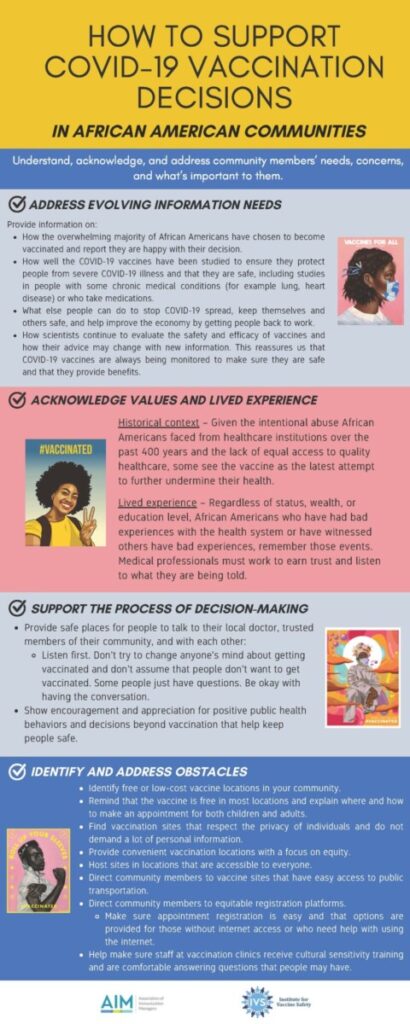
Of course, our most familiar experiences with ID death now come from the ongoing COVID-19 pandemic. Similar to death from both HIV/AIDS and Ebola, there is an element of fear. But unlike HIV/AIDS, Ebola and COVID deaths often times couldn’t be planned (speaking to HIV after the virus was identified and could be tested). There is a sudden finality to it, with people succumbing very quickly after exhibiting symptoms. There is little time to make arrangements, and no time to alert all loved ones. At points, there were no physical goodbyes, no after-death rituals, and very little closure. If you had not lived through the HIV/AIDS crisis, these events were so new and jarring. Regardless, with each disease, it never gets easier. While noncommunicable diseases are the most often causes of death, I’m afraid the future will hold more infectious disease outbreaks. This means thinking about how to handle death with both old and new challenges.