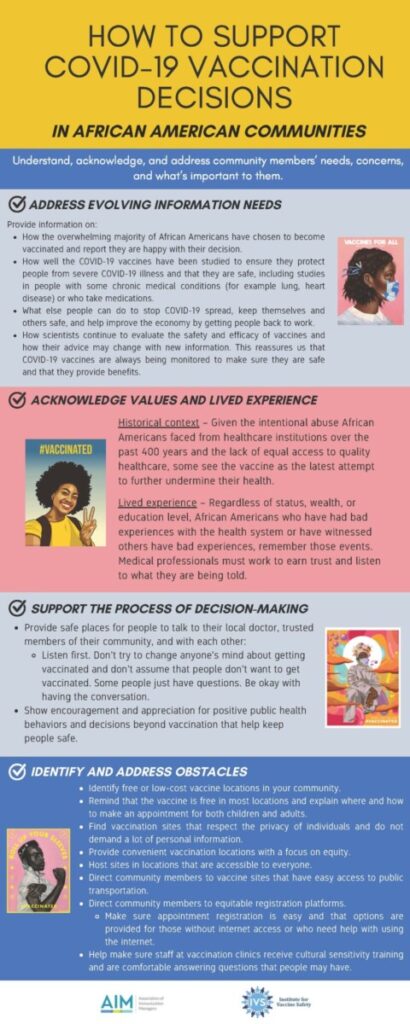
This week, Susan Channa discussed the importance of proper communication between public policy experts and the United States population and several ways one can be an effective communicator. One issue that stood out to me was how much our country’s government and experts struggled to communicate effectively with the US public.
Susan Channa gave clear pointers on how to communicate effectively. Advice such as: Be quotable, deliver key messages, deliver shorter answers, correct misstatements and raise questions yourself. Also, be concise, clear, and compelling and focus on three key messages. This advice made much sense. However, our country and its institutions often failed to follow this advice. Whether it was the CDC, which often released long form and confusing tweets, or President Trump/Biden, whom both have made contradictory statements from public health experts, our country and its institutions have a big problem regarding effective communication.
As we move to a more digital age and an age where public health issues are becoming more and more politicized, what is the best way to move forward so that Americans can receive effective communication? Perhaps the CDC needs more funding to hire better social media experts/training. Maybe public health experts can be given a status and protections that allow them to be more independent, like certain judicial positions in our country.