This week’s readings about end of life palliative care decisions and the struggle of their authors to morally define and establish ethical norms left me thinking about the recent media coverage of Britney Maynard. This past fall, it was difficult to walk into a grocery store without seeing Maynard’s face splashed across a tabloid or lifestyle news magazine cover. Brittany Maynard was a 29-year-old woman diagnosed with terminal stage IV glioblastoma multiforme brain cancer in January 2014. After her initial surgical treatment proved unsuccessful and her tumor returned, Maynard decided to forgo additional treatment of chemotherapy and radiation. According to her editorial for CNN, Maynard and her family reached the conclusion that all remaining treatments could not save her life and would destroy the months she had left to live. Maynard instead chose to establish residency in Oregon in order to gain access to a dosage of lethal barbiturates under Oregon’s Death with Dignity Act, passed and put into effect in 1997.
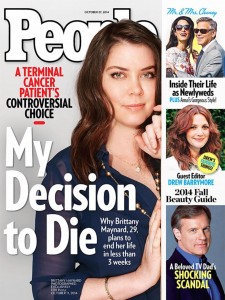
People Magazine Cover October 27, 2014. Digital image. Daily News. New York Daily News, 15 Oct. 2014. Web. 28 Feb. 2015. <http://www.nydailynews.com/life-style/health/terminally-ill-brittany-maynard-graces-people-cover-article-1.1975440>.
This law allows competent adults with a physician-diagnosed terminal illness the right to request lethal prescription drugs and use them to die should they voluntarily wish to do so. Individuals cannot qualify for the drugs solely based on age or disability status, nor can they receive them if they are deemed to have a psychological or psychiatric disorder, such as depression, that could infringe on their ability to make an informed decision about death (Oregon Death with Dignity Act). Once a person has received their prescription, they can choose to use or not use the medication at will. The law still forbids physicians from ending a person’s life in patient assisted suicide through “lethal injection, mercy killing or active euthanasia” and protects the patient’s death (should they choose to use their prescription) from being classified as “suicide, assisted suicide, mercy killing or homicide, under the law”. Brittany chose to end her life surrounded by family members on November 1st, 2014 by ingesting her prescription.
Brittany’s passing left me unsettled and I realized that Beauchamp and Childress and Thomas et al. do little to provide a moral code for judging end of life cases. Their writings detail the necessity for evaluating morality on a case-by-case basis for end of life decisions. Their frameworks for “killing” versus “letting die” and “active” versus “passive” measures explain the beliefs of the medical profession, but they decline to confirm or deny that these frameworks are logical or morally right. On the other hand, Mcintyre, in her discussion about the principle of Double Effect, makes it clear that she would support “deliberate hastening of death” in circumstances where it could “relieve great suffering” (72).
Nevertheless, a decision like the one made by Maynard makes us uncomfortable because of preexisting personal convictions and values that differ beyond the “common morality” we generally use to evaluate ethical situations. Diversity in faiths and upbringings will always create minute differences in the value and purpose of physical life. As Beauchamp and Childress say, it’s not so much what causes death that results in the debate of whether a death is unjustified a “killing” or justified as a “letting die”. They state: “The validity of the authorization—not some independent assessment of causation—determines the morality of the action.” (Beauchamp and Childress 177). Different backgrounds mean people will place validity in the hands of different individuals.
Some may place the validity of the authorization of death only with god, while others may believe it lies with the ill individual alone. In the case of Brittany Maynard, I personally believe that the acceptance or disagreement with Maynard’s decision and Oregon state law comes down to the sanctity of life versus quality of life debate that Thomas et al. describe (210). Those who believe that quality of life is more important than the sanctity of life will choose to honor the principle of autonomy over the non-maleficence/beneficence of prolonging life. And, those who choose sanctity of life as more important will see the prolonging of life as an act of beneficence that is more important than personal autonomy in Brittany’s case—regardless of Oregon law.
Works Cited
Beauchamp, Tom L., and James F. Childress. Principles of Biomedical Ethics. 7th ed. New York: Oxford UP, 2013. Print.
“Death, Dying, and Euthanasia.” Well and Good: A Case Study Approach to Health Care Ethics. 4th ed. Peterborough, Ontario: Broadview, 2014. 208-14. Print.
Maynard, Brittany. “My Right to Death with Dignity at 29.” CNN. Cable News Network, 02 Nov. 2014. Web. 11 Feb. 2015.
Mcintyre, Allison. “The Double Life of Double Effect.” Theoretical Medicine and Bioethics 25.1 (2004): 61-74. Web.
United States of America. Oregon Health Authority. Public Health. The Oregon Death with Dignity Act: Oregon Revised Statutes. N.p., n.d. Web. 28 Feb. 2015. <http://public.health.oregon.gov/ProviderPartnerResources/EvaluationResearch/DeathwithDignityAct/Documents/statute.pdf>.
This is a very thorough and great analysis of Brittany Maynard’s decision to end her life. With the overwhelming support for her decision, perhaps many more states will follow Oregon’s decision and allow patients in positions like Brittany’s to end their lives as well. I think with Brittany’s case, many considered it morally permissible because it appeared in the press to be a completely autonomous and informed decision she made. My concern with end of life opportunities like Brittany’s though, is that there may be situations where people’s autonomy is compromised. Perhaps a patient feels very pressured by a spouse or family members to end his or her life, being seen more as a burden than a person making an autonomous choice. I think with an issue like end-of-life prescriptions ethicists, as well as law makers, aim to be very cautious because every situation is different and some may have the potential to be morally compromising to patients.
I agree with Carolyn that Beauchamp and Childress do not do a concise job of coming to a decision about the morality behind “letting die” vs. “killing.” Of course, it is a difficult line to draw, and may be circumstantial. In cases where an individual cannot make an autonomous choice, I think injecting that individual and allowing for them to die is definitely morally wrong. In Brittany’s situation, she does have the autonomy to choose to end her life, however she is doing so in a very active way. For me, the sanctity of like morally overrides the desire to die, which is why I also think that suicide is not morally just. There is a difference between something being legally ok and something being morally ok. In this situation, she is choosing to go to a legal clinic to take something that will put her out of her pain for good. So technically it is legal, however in my eyes it is still morally wrong . I do agree with Carolyn that it comes down to what you value most, sanctity of life or quality of life.
This was a very thorough explanation of Maynard’s medical situation and decision to end her life. I believe that people should be able to choose a dignified death. Unfortunately, death is a part of life. Maynard minimized the harm that would be done to her and her loved ones by choosing to dignified death. She would have physically suffered from her illness and been long gone before her body gave out. This was a difficult decision to make, but it gave her the opportunity to reclaim her dignity and die in peace. It also saved her friends and family from watching her suffer. My only issue is that every case is not like Britney’s. People may feel pressured or have other motives for ending their lives. And as horrible as it sounds, this may put a great financial burden on the family. How does this play into life insurance policies, financial debt, and other things that will continue after that person is gone?
I actually think the opposite is true! I think the financial burden on the family would be less due to the high cost of life preservation services. Patients should have the autonomy to decide how to end their terminal illness process. In this process, today’s medical technology can preserve and extend life at all costs. Patients can be forced to continue breathing and hearts can be resuscitated to continue beating. However, these life-sustaining measures are bought with a patient’s dignity. Is it not more humane to allow a patient suffering from terminal cancer to end her life peacefully surrounded by family, than to continue sustaining her life via painful medical procedures until her body finally gives up?