In Howard Brody and Eric Avery’s Medicine’s Duty to Treat Pandemic Illness: Solidarity and Vulnerability, they conclude physicians have a duty to treat pandemic illness because there is “no single ethical foundation for a duty to treat that would be commensurate with the needs posed by an emerging infectious disease pandemic” (Brody, 42). While I respect and understand the reasons behind their conclusion and appreciate their consideration to individual commitments and social values, I do think they fail to speak to some other ideas in question such as, what does it mean to be a physician?
The authors claim “by announcing to the community they are practitioners of medicine, physicians implicitly accept and undertake these duties,” (Brody, 40) but this raises the fundamental question of what it means to be a physician. As mentioned in the article, some physicians reacted to the assumption of their duty to treat with thoughts such as “Wait a minute—I never signed up for this” (Brody, 42). This got me wondering, why do people become physicians? Is it for the “awe of discovering the human body, the honor of being trusted to give advice, the gratitude for helping someone through a difficult illness”, for the prestige of the “Dr.” title, for the financial means it provides, or for another reason (Ofri)? Whatever the reason may be, these few listed options make me question whether all physicians go into medicine so that they may “help people” as many of my pre-med colleagues would say. There are many different professions and roles people can take on to help people, and perhaps, people take on the role of physician for the science rather than the people-aspect. If that is the case, we could argue that they indeed did not “sign up for this (referring to endangering oneself for the sake of the patient).” That being said, “the tradition of the American Medical Association, since its organization in 1847, is that: ‘what an epidemic prevails, a physician must continue his labors without regard to the risk to his own health” (Daniels, 37). So, in a way, physicians should know what is expected from them. However, I acknowledge reality is not so black and white. Some physician specialties to consider are: anesthesiologist, cardiologist, dermatologist, endocrinologist, family medicine, forensic pathologist, hematologist, infectious disease specialist, neurologist, oncologist, psychiatrist, radiologist, sleep disorder specialist, sports medicine specialist and more. There are so many different types of physicians and each specialty has different degrees of exposure to hazard. I wonder if the strict adherence to the duty to treat would deter people from entering certain specialties innately more prone to hazards involved with pandemics (ie. infectious diseases, etc). There are many frustrations that come with the role of a physician including the short amount of time allotted to visiting patients and the documentation and technical duties that come with patient visits.
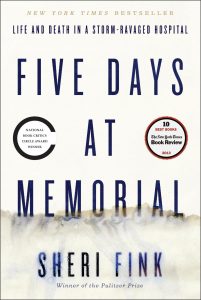
To read more on the debate over duty to treat, I recommend the book, which comes to mind called Five Days at Memorial by Sheri Fink. It is a book about Hurricane Katrina wreaking havoc and sending hospitals such as Memorial into a state of crisis. While some healthcare professionals flee the storm and leave behind patients, others stay at the hospital and continue giving care, working till exhausting and continuing despite being understaffed and having limited resources. This parallels the treatment of pandemics in that health care professionals put themselves in harms way.
I also recommend checking out this article, “Duty to Treat and Right to Refuse”, by Normal Daniels: https://www.jstor.org/stable/3562338?seq=1#page_scan_tab_contents
While I hope physicians take on the duty to treat no matter what, I ultimately still see the role of treating during pandemic as supererogatory. I see these healthcare workers as humans first, then physicians. If they want to prioritize their own health, family, or something else, they should be able to do that.
Citations
Beauchamp, Tom L., and James F. Childress. Principles of Biomedical Ethics. 7th ed. New York, NY: Oxford UP, 2001. Print.
Brody, Howard, and Eric N. Avery. “Medicine’s Duty to Treat Pandemic Illness: Solidarity and Vulnerability.” Hastings Center Report. The Hastings Center, 15 Jan. 2009. Web. 16 Apr. 2017.
Fink, Sheri. Five Days at Memorial: Life and Death in a Storm-ravaged Hospital. New York: Broadway, 2016. Print.
“Medical Specialists – Types of Specialists.” WebMD. WebMD, n.d. Web.
Ofri, M.D. Danielle. “Why Would Anyone Choose to Become a Doctor?” The New York Times. The New York Times, 21 July 2011. Web. 17 Apr. 2017.
Thomas, John E., and Wilfrid J. Waluchow. Well and Good: Case Studies in Biomedical Ethics. Peterborough: Broadview, 1987. Print.
Hi Pamela! I enjoyed your post and I agree with your thoughts. As a student on the pre-med track myself, I often ask similar questions to ensure I am pursuing this field for the “right reasons”. I agree that the excitement for science and human anatomy must play a role as there are numerous other professions that help just as much, if not more, than physicians. For example, if my primary goal and passion was to help people (and I wasn’t super excited about human anatomy), I could teach or start a nonprofit. Many students on this track decide blindly without realizing the other obligations that come with this challenging position.
While I agree that these acts are supererogatory for a typical physician, they are not an option for those who specialize in emergency medicine or infectious disease, as these physicians have purposely signed up with the knowledge that they could be harmed in the process. If they were not obligated, EMTs would avoid patients with influenza and Emory would’ve never treated the Ebola patients. The risks are so high, but because that is their specialty, I believe they are obligated to help. However, if a sports medicine doctor or a psychiatrist decided to treat cholera patients in Haiti, that would be supererogatory since it is external to their job description.
It almost seems like physicians in different specialties are so different that they should be considered different careers. I wonder, also, if treating a patient outside of your specialty can do more harm than good – putting not only yourself but your patient in danger. Would it be supererogatory in this case, or just plain harmful?
As we know, doctors are not the only professionals with a duty to help and/or rescue. Think of firefighters. While searching the web on this topic, I stumbled upon an interesting article. A volunteer firefighter in Waco, TX suggested the beginnings of a proposed bill to allow emergency responders, such as paramedics and firefighters, to carry firearms on duty for self-defense. Let’s think about this for a moment: a duty to help coupled with a duty to harm if threatened. It’s an interesting paradox. As the volunteer firefighter states, “Being licensed to carry while on a call or during a fire department function is no different than having the need to carry while you’re a private citizen at home. Those unfortunate situations can arise at any time, even on fire calls. Even during a fire call, there’s sometimes a heightened threat there” (Smith, 2017). I disagree with his first statement as there is a clear difference between being on duty and being at home which is the duty to rescue. While I understand the need for protection, I wonder how these challenging principles – duty to rescue another vs. duty to rescue themselves – balance in these situations.
To tease this out, if self-defense is justified for a medical provider, I wonder who, if anyone, would be able to treat a harmful person. For example, take a patient with a severe mental illness. They are violent and a danger to themselves and others. Are the physicians still obligated to help then? Or are their acts supererogatory even if mental illness is their specialty? Can we separate these duties – for example, leave the risks to a security guard and use the physician when the patient is stable? These are tricky questions and I look forward to hearing your thoughts!
Smith, C. (2017). Bill would let firefighters, EMTs carry guns on duty. Waco Tribune-Herald. http://www.wacotrib.com/news/city_of_waco/bill-would-let-firefighters-emts-carry-guns-on-duty/article_840165fb-01c1-5b19-a48f-7701723e79aa.html
Hey Pamela,
I appreciated the points you focused on, especially when you mentioned seeing physicians as humans first. One thing I believe needs to be addressed is how as a society, we sometimes hold unrealistic expectations of physicians. While physicians are held to a high standard, we should remember that physicians make mistakes just like other professionals.
In terms of physicians providing treatment for pandemic illnesses, it rests on the assumption that there will still be physicians available after the event has subsided. However, suppose there is a hypothetical situation, and that every physician that treats a pandemic illness will get infected as well. If all physicians in an area treat a pandemic illness, then there will be no one left to treat other illnesses that could arise, which goes against the utilitarian theory of producing the maximal benefit for everyone involved. That is why I propose a situation similar to the one you suggested, in that it may be obligatory only for some individuals to provide care in potentially harmful situations, such as EMT workers. This is due to the fact that they were aware of the risks involved prior to completing their training, however, they chose to stick with the profession nonetheless. If residents were aware of the risks involved with being a physician, then that raises another set of questions that should be asked.
Citation:
Beauchamp, Tom L., and James F. Childress. Principles of Biomedical Ethics. New York: Oxford UP, 2009, 2013. Print.
Thomas, John E., Wilfrid J. Waluchow, and Elisabeth Gedge. Well And Good: A Case Study Approach to Health Care Ethics. N.p.: Broadview, 2014. Print
Hi Pamela,
I definitely agree with you that doctors of different specialities assume different levels of risks and responsibilities when there is an pandemic. I don’t believe physicians, even those specializing in fields that could help the pandemic, are obligated no matter what to help. In doing some light research to support my argument, I came across a paper by Daniel Sokol discussing his views on the responsibilities during an epidemic. He brought up many good point that involved weighing the risks that a physician would take with the potential to actually make a difference. A really interesting point that Sokol made was that he believed patients also had a duty to doctors: “Patients too have a duty to care for healthcare workers. Part of this duty is not to require doctors to transcend the bounds of reasonable risk during treatment and to respect and acknowledge their roles outside the realm of medicine” (Sokol 1240). It’s really interesting to me because I feel like we always discuss the duty of doctors to patients, but not the other way around. If the risk to a physician, and the people he interacts with (like his family) are too high, do you think a patients has a duty to let the doctor walk away?
Sokol also had a great analogy that really brought his point, and my opinion, home:
“If a swimmer in an isolated but supervised beach starts to drown 50 meters from the shore, the lifeguard may reasonably be expected to attempt a rescue. This, after all, is the lifeguard’s duty as a qualified professional. If, however, the person is drowning 2 miles out and is surrounded by a school of hungry, man-eating sharks, then one cannot expect the solitary lifeguard to dive among the sharks to save the swimmer, even if that means the swimmer will certainly die and even if the lifeguard has a small chance of saving him or her (at great personal risk)” (Sokol 1240).
If a doctor is in a place where the resources are extremely limited and the pandemic is widespread, does he have an obligation to stay and help if it brings him great risk? I don’t think he does. I agree that if there are enough resources then a doctor should help, but I begin questioning this obligation if its clear that they alone can’t help, and are just bringing greater risk to their own safety. This starts to bring about the question in our final paper: Are countries obligated to provide medical assistance to non-citizens? If there are more resources in these places with pandemic, it will make the aid of doctors less supererogatory because their help could actually make a huge difference, and they’re safety would be less compromised.
Work Cited:
Sokol, Daniel K. “Virulent Epidemics and Scope of Healthcare Workers’ Duty of Care.” Emerging Infectious Diseases 12.8 (2006): 1238–1241. PMC. Web. 22 Apr. 2017.
Hi Pamela,
I loved your post! You touched on a lot of key ideas about the complexities involved in being a physician. It made me think about my cousin, who is a UN doctor that went to Sierra Leone to treat ebola during the pandemic. When he was assigned the position, initially a lot of our family members objected due to the potential risks, especially with the fact that he has a wife and two kids. But in the end, he saw it as a way to solve a very serious issue, and outlined the fact that if it doesn’t get treated or if people don’t volunteer to take it up, then the problem will just continue to grow and then it will become ‘our problem’. I think this example and the one that you brought up brings up a very big idea, which is that physicians enter the field for different reasons, and I don’t think that they should be looked down upon or be considered less of a physician because they put themselves as a priority, but I do think that being that they went into the job, they understand that there are certain aspects of the job that might arise to where they might be put in a potentially hazardous situation. It makes me think of people in the police force or the army, they know that their job is potentially dangerous, yet they do what they do because it’s their job, and in order for the job to carried out to the best of their abilities, they might have to put themselves at risk. I feel like its sort of the same with physicians, to a certain degree
Hello Pamela!
I really liked your post. It reminded me that I need to start thinking of this question for myself (like many other people that are taking this class, I am also pre-med). I think the strait forward answer is simply someone who takes in sick people and attempts to make them better. The question – why do people become physicians? – you’re alluding to, on the other hand, is something much harder to pinpoint. None the less, by becoming a physician you take on the responsibility that comes with the title “Doctor”. I agree with you that they do not need rise to every occasion. There are limitations to what humans can do~ Society and logistics often complicate logical responses.
The question I ask in return is: Do the motives behind the doctor matter if the result is positive?
Thanks,
Alex