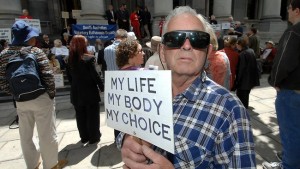
When looking at physician-assisted death from a legal perspective, most governments would deem it is as wrong; there are only 5 out of the 50 states in the Unites states that allow such a practice. However, despite the law, from a moral standpoint, someone of full cognitive capabilities choosing to die should only be viewed as right. The reason for this goes back to the moral principles of autonomy and moral status.
As an autonomous person your, “personal autonomy encompasses self-rule that is free from both controlling interference by others and limitations that prevent meaningful choice such as lack of understanding” (101). With autonomy you are capable of self-government as long as nothing is impeding your choices like an illness or a lack of understanding. I know I just mentioned illness and one might argue that individuals that opt to die by the hand of a physician are ill and cannot make that choice autonomously. To that argument, I would say it does not apply in situations where someone is fully in control of all cognitive capabilities but also happens to have a terminal disease. Also, it is important to distinguish between illness and disease. It is possible for one to have a disease and not be ill. Essentially illness is a subjective state of being that manifested from a disease. While a disease is the presence of a pathological systemic issue that can result in illness (Illness). Thus, when someone is merely diseased but not yet ill, their autonomy is not hindered by their mental state. In fact, in their capable mental state they are making the decision to not get to a point where disease transitions into illness. At that point, the physician has a moral obligation to respect a patients autonomous decision to avoid suffering leading up to their inevitable painful death.
In the stipulations for a physician’s assisting someone’s death, it mentioned that there should be a voluntary request and unacceptable suffering (Beauchamp 184). The aforementioned two stand out because they indicate a person’s consent as well as an indication they do not desire the quality of life that lay ahead. Beauchamp and Childress claim:
If a person freely authorizes death, making an autonomous judgment that cessation of pain and suffering through death constitute a personal benefit rather than a setback to interests, then active aid-in-dying at the person’s request involves neither harming nor wronging (182).
There is not moral wrongdoing when someone is of sound mind and sees more benefit in ending their life early instead of dragging it out to end with suffering. From the physicians perspective it is wrong of them to knowingly leave a patient to be in pain or a low quality of life against their will. Take for example to case of Sue Rodriguez, she felt the law compelling her to stay alive through her debilitating disease was hindering her rights to life, liberty, and equal protection of the laws. However, her requests were denied on the grounds that suicidal practices were not legal. That stated, those previously mentioned facts of the case are about laws and not morals. Morally, a physician has a duty of non-maleficence and a need to respect patient autonomy, if they are capable. A patient being forced to live in pain is a harm, which is keeping them from the goods of life. This may be part of the reason why when Ms. Rodriguez took her life neither of the parties that assisted her was punished. Regardless of what the law says, it’s the individual who should be in control of their life and how they want to die if diagnose with a fatal disease.
P.S.
One other thing that interested me outside of the moral standing of physician-assisted death was the discrepancies in judgment of the Kevorkian case. Most bioethics writers have condemned Dr. Kevorkian but the physician and friend in the Rodriguez case were not. Are these not very similar incidents? I am curious to know what people think.
Works Cited
Beauchamp, Tom L., and James F. Childress. Principles of Biomedical Ethics. New
York: Oxford UP, 2009. Print.
Illness, Sickness, and Disease | Primer on Public Health Population.” Illness, Sickness,
and Disease | Primer on Public Health Population. The Association of Medicine
Canada. Web. 13 Mar. 2015. < http://phprimer.afmc.ca/Part1-TheoryThinkingAboutHealth/Chapter1ConceptsOfHealthAndIllness/IllnessSicknessandDisease>.
Thomas, John E., and Wilfrid J. Waluchow. “Case 8:3 Sue Rodriguez: “Please Help Me
Die”” Well and Good: A Case Study Approach to Biomedical Ethics. 3rd ed. Peterborough: Broadview, 1998. Print.
Although I am unsure where my beliefs lie in terms of aiding a patient’s suicide, I do agree with many of your points. If a patient is of stable mind and wants assistance in ending their life because they are suffering, I see how it could be maleficent to allow the patient to continue to suffer. However, one thing you did not address was the slippery slope of what could happen if we allow for physician-assisted suicide. How would we create boundaries for who can request assistance and who cannot? Should we be afraid that if this were to become legal there would be persuasion and suddenly cases of euthanasia that would not have occurred otherwise? My fear is what would come next if we were allow certain patients to be assisted in dying.
Hi Danielle, you are right I did not address the slippery slope argument/opposition. I feel that the stipulations that would need to be in place would definitely need to pertain to the person having some kind of terminal illness or degenerative disease that is inevitable so it would not just be giving people license to sign up for suicide on a whim. Additionally, physicians should not be coercing or suggestive of these measures, merely facilitators, it should be the patient that comes to the conclusion of wanting to end their life and not the physicians place to bring them there. I think its valid to have fears for what could occur to let patients to die, but at the end of the as I said is it really our place to cause people to live out their illnesses and suffer for the sake of having them still be alive?
Ugochi,
To answer your last question, we do not know how involved the doctor was in Sue’s life before she/he decided to assist in Sue’s suicide. One of the reasons why Dr. Kevorkian is so heavily criticized is because he helped Janet Adkins commit suicide without having any real history with her and without consulting with her extensively about her medical situation. He just helped her kill herself without any question or hesitation. Whereas with the unidentified doctor who helped Sue, we do not know how long of a relationship the doctor had with Sue. For all we know, this doctor and Sue’s friend “Mr. Robinson” both could have tried to convince Sue to not commit suicide for an extensive amount of time. Perhaps the doctor arranged for Sue to meet with psychiatrists or tried other alternatives to help her ease her worries about her prospects with ALS before they agreed to help her end her life.
In the interview with Dax Cowart that we have to read for this coming week, the following question was asked: “When is it okay [for the doctor] to say, I agree with you. You (the patient) can call an end to [your life].” It is okay for a doctor to agree that the patient can call an end to their life once the doctor has exhausted all possibilities that could have provided comfort to that patient and spent extensive time (at least a few months) care for the patient. For all we know, Sue’s doctor and friend may have done just that unlike Dr. Kevorkian. I do find it odd that Sue’s suicide assistants weren’t punished under section 241 at least because they blatantly violated every aspect of the code.
The importance of hope in medicine cannot be undermined. Why do we visit doctors? We go to doctors expecting to find a cure for an illness. We try to seek relief, words of comfort, and signs of assurance that our medical case is curable. Most importantly, we go to doctors to seek hope, which arises when patients feel that something can be done. On the other hand, when patients are informed that they have a terminal illness, their depressive emotions and miserable mood will affect their abilities to make rational decisions. They might ask to terminate their lives out of fear of pain, becoming disabled or ending up to be a financial burden on their loved ones. The ability to create and maintain HOPE is the main theme of health care. If the disease is terminal, then what the patients need is help, as well as, compassion and not a medicine or a lethal injection to terminate their life. Aiding in helping patient to commit suicide is not the role of doctors.
I’ve always thought that the role of a doctor is to help, cure, manage pain, and provide medical care but not terminating the patients’ life in the name of “dying with dignity”. If competent patients have the right to decide the termination of their life then the surrogates of disabled patients should have the right to decide the termination of the life of the disabled patients they represent. This will lead to a slippery slope that will not only be uncontrollable but will also force other vulnerable patients to command assistance in suicide in order not to be a financial burden on their families. If PAS is legalized, the value of human life will decline, medical care in hospice and other medical care organizations will decrease, values, cultures, religions, beliefs will all be altered and virtuous responsibilities of the family members towards their elderly and terminally sick parents will weaken. In my opinion, doctors in the utmost may stop futile treatment that will elongate the suffering of terminal ill patients and then let nature take its course. Autonomy has to be respected under certain circumstances but not when asking doctors to aid patients’ decision to commit suicide. I’m aware that, “suffering and loss of cognitive capacity can ravage and dehumanize patients so severely that death is in their best interest” (Beauchamp and Childress p. 184), but I equally know that what makes us human is being humane in helping others, caring for them when they need our help and not help them kill themselves. Many patients commit suicide on their own and they do not need the aid of a doctor for their actions. Let the doctor remain as a symbol of medical care provider and not as that of a life terminator.