Dilemma:
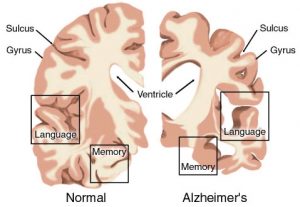
If you were the head of a nursing home and a researcher approached you and asked if she could use your patients as subjects in her study what would you do? Now suppose that your nursing home is for individuals suffering from Alzheimer’s disease. Would your decision on whether or not to allow your patients to participate waiver? In Case 3.1, Ann Wilson is the director of St. Mary’s Nursing Home, which cares for those suffering from Alzheimer’s disease. A researcher, Dr. Selleck, contacted Ann about her need for individuals suffering from Alzheimer’s who would be willing to participate in a trial to test a new drug that supposedly slows the progression of Alzheimer’s disease. Dr. Selleck asked for Ann’s permission to use her patients as potential subjects after explaining that she would only choose patients to participate if they had written consent, a relative’s written consent, and no one on the health staff had objections to the patient participating. Ann decided not to allow Dr. Selleck to use her patients at the nursing home (Thomas, et al. 116-124). Was Ann right to make this decision on behalf of her patients?
Discussion:
Ann’s decision raises the question of whether Ann is protecting her patients, or doing a disservice to them by denying the patients the opportunity to participate in the study. By making a decision on behalf of a patient without consulting them, Ann is violating the patient’s right of autonomy. However, the amount of autonomy an individual deserves in a situation is based on their competency. By law, someone is either considered competent or not competent. After further research, I found the criteria lawyers follow to classify someone into one of these two categories. As you can see in the article, the steps of classifying an individual into one of these categories is very black and white. Legally there is no in-between, while in reality there are several degrees of competency (Israel). This case deals with the two moral principles of autonomy and nonmaleficence. The only way to “solve” this case is to find a balance between these two opposing principles. How can one respect the autonomy of a patient while also protect them from experiencing harm?
I do not agree with Ann’s response in the case presented. I think that the best response in this situation would be to allow the patients to be interviewed as potential subjects in the study. This gives the patients the option to make the decision of whether or not they want to participate for themselves. However, in order to protect the patients, I would only allow those who are considered competent to participate. In addition, I would ask the patients and their relatives what they want as a way of respecting their autonomy, but also let the health care staff contribute to the conversation to decide whether or not the patient would be safe to participate in the study. If the risk of harm is too high, I would allow the health care staff’s opinion to outweigh the patient’s autonomy. If the patient is not competent I would protect them from harm rather than respect their autonomy. However, if the patient was considered competent, as in Case 3.2 where Simon competently chooses to not receive electroconvulsive shock therapy, I would respect the patient’s autonomy (Thomas, et al. 124-131).
Works Cited:
Israel, Laurie. “Elder Competency – When Can You Make Your Own Decisions?” IVKDLaw. IVKD Law, 2010. Web. 20 Jan. 2017.
Thomas, John E, et al. “Case 3.1: Research Involving Alzheimer Patients” Well and Good: Case Studies in Biomedical Ethics, Broadview P, 1987.
Thomas, John E, et al. “Case 3.2: Nonconsensual Electroconvulsive Therapy.” Well and Good: Case Studies in Biomedical Ethics, Broadview P, 1987.
Hi Morgan!
Like you, I agreed that the patients right of autonomy should be respected and that their decision to take part in the study or not should be respected. In addition, I connected with the part of the discussion that mentioned that such elderly feel privileged to participate in such crucial scientific research and believe that studies like this one give their lives purpose. I also felt that the part of the discussion that emphasizes the necessity of such studies provides further reasoning for the participation of individuals with alzheimers in the study.
That being said, I felt that there are a couple areas of your discussion that may result in a gray area. In your discussion, you mention that subjects should participate in the study as long as the risk of harm is not too high. What constitutes a high risk of harm? How is harm measured? In addition, you mentioned that the wishes of they patient, their family members, and the hospital are considered when making a decision about the competency of the patient and their ability to participate in the study. What holds more weight? The patient, their family, or the hospital? Does this differ from patient to patient?
Noa,
Thank you for your comment! I am writing to respond to your questions regarding my proposed plan for allowing patients to participate as potential subjects in the Alzheimer’s study. In my plan, I discuss how “if the risk of harm is too high, I would allow the health care staff’s opinion to outweigh the patient’s autonomy.” If a study includes possibilities of death, possible worsening symptoms of Alzheimer’s, and possible severe distress to the patient, I would consider the study to be of high risk. The level of harm in a study would be measured by reports conducted by the health care staff and patient. For example, after a session with the research team, a health care staff member and patient would discuss whether the activities the patient was asked to perform in the study made the patient’s symptoms worse than on a daily basis (Human Subjects Protection Program). If the symptoms are worse than the patient would encounter on a daily basis, then the risk of the study would be considered “high”.
To address your other concern as to whether the wishes of the patient, their family, or the health care staff holds more weight than the other, I would respond that it depends on the patient’s competency and the possible risks of the study. As stated in my blog post, if the risks of the study are considered high, then the health care staff’s decision would weigh more than the wishes of the patient and their family. If the study is considered low risk and the patient is considered competent or semi-competent, meaning their competency fluctuates throughout the day, the wishes of the patient and their family would hold more weight than the health care staff. In essence, I would attempt to respect the patient and their family’s autonomy in the matter, unless their possible decision could cause the patient severe harm, such as a high risk study.
Thanks for your thoughts. I hope this answers some of your concerns.
Works Cited
Human Subjects Protection Program. “Risks to Research Participants.” Human Subjects Protection Program – Policy Manual. University of Louisville, n.d. Web. 31 Jan. 2017.