The surgeon in this case is faced with legal and moral obligations to the woman and her family, and it is important to understand the law and the necessity of effectively measuring competence, regardless of how the surgeon feels about the woman’s decision.
From a strictly legal standpoint there is very little that the surgeon can do to force the woman to accept a surgery, even if he feels her decision to refuse care is medically or morally irrational. An example of a Supreme Court case that illustrates this point is Lane v. Candura in which a woman refused an amputation that would save her life. The woman’s daughter attempted to gain the rights of guardianship, and by extension right to force her mother to receive the amputation, but the court stated that the woman had the right to refuse treatment and was fully competent to do so. While the woman’s child in case 1.1 is not seeking full guardianship and control over his mother like the child in the Supreme Court case, and the specific reasons for refusing further treatment are somewhat different between the two cases, there is a strong parallel between these cases. In the Supreme Court decision, the woman was allowed to refuse the amputation surgery, and it seems that the woman in case study 1.1 has a similarly justifiable ability to refuse treatment.
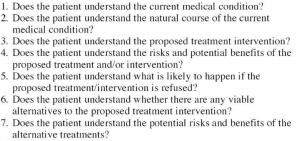
Regardless of the law, it is a good idea for the surgeon to perform a comprehensive analysis of the woman’s competency in order to avoid oversight that might clear up a moral ambiguity or be necessary to protect himself in the event that the woman or her family sues him. Dr. Leo’s list of questions provided in his article titled “Competency and the Capacity to Make Treatment Decisions” provides a solid list of questions that can be used to determine a patient’s ability to understand the nature of the treatment in question and the results of their decision.
Based on the information presented in the case, the woman appears to be able to understand her treatment options and the severe likelihood of death if she chooses to forego any addition medical care.
With this in mind, the main cause for concern about the woman’s competency is ensuring that there aren’t any controlling factors, especially relating to the pain and frustration she is feeling, or potential animosity towards her family. The surgeon might want to ask about the woman’s pain levels, her relationship with other family members, and what she is most frustrated by. It might even be appropriate to ask some of these questions after the respirator has been removed since it can cause discomfort and frustration. It could also be helpful to attempt to regain the woman’s trust in surgeons by trying to connect with her at a more personal level.
If the woman remains adamant, especially if pain levels are low and she is not feeling pressured or upset by her family, then the surgeon does not have many options but to allow her to refuse treatment and possibly face an eventual suit from the son.
Citations:
Leo, Raphael J. “Competency and the Capacity to Make Treatment Decisions: A Primer for Primary Care Physicians.” The Primary Care Companion to The Journal of Clinical Psychiatry 01.05 (1999): 131-41. Web.
Hey Jack,
While I do think that this is a troubling situation with no clear answer, the physician may have been able to accomplish more than what was stated in the case. Based on the “Disclosure” section from Principles of Biomedical Ethics, physicians are obligated to disclose a certain set of information to patients so that they can accurately make a decision. One of those pieces of information is the physician’s recommendation. Although Marie can state her decision not to have surgery, the physician can state his professional opinion in the matter, rather than what the medical literature states should be done. This process accomplishes two things: (1) it allows the patient to gain medical advice from someone who has more experience and (2) establishes a personal relationship between the physician and the patient. If the patient learns information about the procedure previously unknown to them, they may change their mind about opting to accept or deny the operation. In terms of the personal relationship, the patient may feel comfort knowing someone is concerned about their well-being. In Case 1.1, the patient adamantly refused surgery when it was discussed with a family member. If concern is expressed to the patient, they may open up to what others have to say.
Citation:
Beauchamp, Tom L., and James F. Childress. “Disclosure.” Principles of Biomedical Ethics. 7th ed. New York, NY: Oxford UP, 2013. 125. Print.
Hi Jack,
In your analysis of Case 1.1 you argued that due to the fact that Marie’s understanding falls in line with Dr. Leo’s principles, she is deemed competent and therefore fit to reject life saving surgery. You cited the Supreme Court Case Lane vs. Candor in which a woman, who was deemed fully competent, refused an amputation and stated that due to the parallels of the case, Marie should have the right to refuse the surgery. That being said, you ended your analysis by saying that external factors such as animosity to one’s family and pain levels should be considered when judging competency. My concern with this argument is a. how do you determine which factors should be considered? and b. at what point do you argue that an external factor has the ability to override a life saving operation. I completely understand why you felt the need to mention the influence of external factors in this case and I think that in doing so you shed light on the difficulty of weighing competency vs. a physicians obligation to his patient, familial concerns, and the concept of a patients best interests.
Noa
I agree that it’s hard to decide which kinds of factors are worth taking into consideration. I mentioned a few examples to touch on the argument that there may be other factors that could be compromising her decisions, and the examples were based on past readings I’ve done or conversations I’ve had regarding the effects of pain or strained relationships on emotion, and how emotional instability can effect decision making. For example one article notes that, “Anterior insula activation is consistently seen inneuroimaging studies of pain and distress…This region has also been implicated in studies of emotion, in particular involvement
in the evaluation and representation of specific negative emotional states… Chief amongst these are anger and disgust” (Sanfey et. al 1756). There are other studies on chronic pain’s effect on decision making, as well as evidence that other negative influences on emotions can, to an extent, lead to “irrational” decision making. There are other influencers, such as the pain medicine, that can have effects on her decision making. Those examples are by no means a comprehensive list of such factors.
In my opinion, there is not enough evidence in this area to make a decision that overrides the patient’s decision. Rather, the caregivers ought to try to ease these discomforts or strains on the patient’s emotional state, partly to ensure that her decision making is clear as possible, regardless of what her decision is.
Citation:
Schultz, Wolfram. “Faculty of 1000 evaluation for The neural basis of economic decision-making in the Ultimatum Game.” Science 300.5626 (2003): 1755-758. Web.