Case 6.1: Two Different Requests to Be Left to Die: John versus John
In Case 6.1a and 6.1b the two cases are compared and contrasted on multiple levels. What stands out to me the most is John’s case of “sanctity”. John is a man of 26 years of age who suffers from the elephant man’s disease, also known as Proteus Syndrome. John is captive on the respirator and urges his conscious decision to end his life and disconnect from the respirator. Many questions arise from paying respect to John’s decision. Should the doctors and his family respect his “sanctity” and allow him to die by his own choice or should others take over and exert control over his life?
John is fully alert, conscious, and in control of his mental faculties and clearly he wants to die. What stood out to me was what the elephant man’s disease was and how it could cause someone to consciously want to die. John has been suffering from this syndrome for 20 years and has gone over 100 operations as a result of uncontrollable tumor growth.
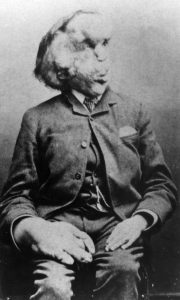
Proteus syndrome is results in abnormal growth of bones and blood vessels, as well as benign tumors on the body’s nerves. This syndrome results in a whole facial disfiguration, as well as physical disfigurement (DermNet). The case is mirrored by the “Real Elephant Man”, an Englishman named John Merrick, who the disease is named after. Merrick was supposedly a “circus performer” due to his physical appearance. However, Merrick had an indomitable spirit in which he utilized his freakish physical appearance and became a popular icon. He was in fact one of Queen Victoria’s favorite performers at that time. In a sense John Merrick’s attitude towards his syndrome is very dissimilar to the John in this case study. In a bigger sense, are two scenarios comparable in bioethics due to similar diseases and symptoms?
According to the physicians, John would most likely live for many years if John continued on life support. However, the question of whether or not John’s autonomy should be respected arises. Is allowing for a patient to live for a few more years morally correct even though the patient wants to die right now? John’s family members were initially very opposed to John’s autonomous decision to end his life. However, after extensive counselling, they accepted his decision. Therefore, the role of the counselor is also very impactful on the family’s perception of the scenario. Could John also be counseled and therefore have a change in his autonomous decision to die?
Now a question arises of how much of an impact can external factors have on one’s decision making, especially in the case of choosing to end one’s own life. For John Merrick, there was popular support in his actions and he was notoriously a figure/icon to many people around him.
Merrick obtained many supporting visits from many different people when he was hospitalized.
In this scenario I would choose to encourage as much positive support for John (from case study) as possible and encourage counseling and social support.
Works Cited
Ngan, Vanessa. “DermNet New Zealand.” Proteus Syndrome | DermNet New Zealand. N.p., n.d. Web. 9 Feb. 2017.
Sheward, David. “The ‘Real’ Elephant Man: A Look at the Life of Joseph Merrick.” Biography.com. A&E Networks Television, 15 Dec. 2014. Web. 10 Feb. 2017.
Thomas, John E., and Wilfrid J. Waluchow. Well and Good: Case Studies in Biomedical Ethics. Peterborough: Broadview, 1987. Print.

Enjoyed the post!
While I do think the physicians should give the patient appropriate time to make a decision, care needs to be taken to ensure that the physicians are not coercing the patient into leading a longer, but less desirable life. From the facts presented in the case, it seems as if John’s condition has impacted his life severely, and may have hampered his ability to live a normal life. As such, John feels as if he would be better off removing the respirator and not living. From the perspective of the physician, questions should be raised as to why John has made this decision. If his current condition has impacted his cognitive abilities, then he may be rendered incompetent, and as such, unable to make decisions. However, if this is a situation John has rationally thought over, then respect should be given to his decision, regardless of if it is in his medical best interest.
Citation:
Thomas, John E., and Wilfrid J. Waluchow. Well and Good: Case Studies in Biomedical Ethics. Peterborough: Broadview, 1987. Print.