Case 6.2: Sue Rodriguez: “Please Help Me to Die”
Introduction
Physician-assisted suicide is one of various types of end-of-life decisions debated in bioethics and legal circles. In this case, Sue Rodriguez has ALS. Once she began to experience deterioration of her abilities, she entertained the possibility of suicide and petitioned the courts for an order “which would allow a medical practitioner to set up technological means by which she might […] end her life.” After the Supreme Court of Canada issued its ruling, she took her own life with the assistance of an unidentified physician. In 2012, Gloria Taylor suffered from the same disease that affected Sue and brought the issue to the forefront of the Canadian public once again (Thomas, Waluchow, & Gedge 214).
The Question / Discussion
Like many of those we have discussed in class, this case presents a question about the morality of the choice of a physician to assist suicide, not directly about the legal issue; setting aside the legal question, which regards social policies and actions of the political community as a whole, if you or I were a physician, would it ever be morally right for us to choose to assist someone to commit suicide? (Lee 213).
Intentional Killing vs. Accepting Death as a Side Effect
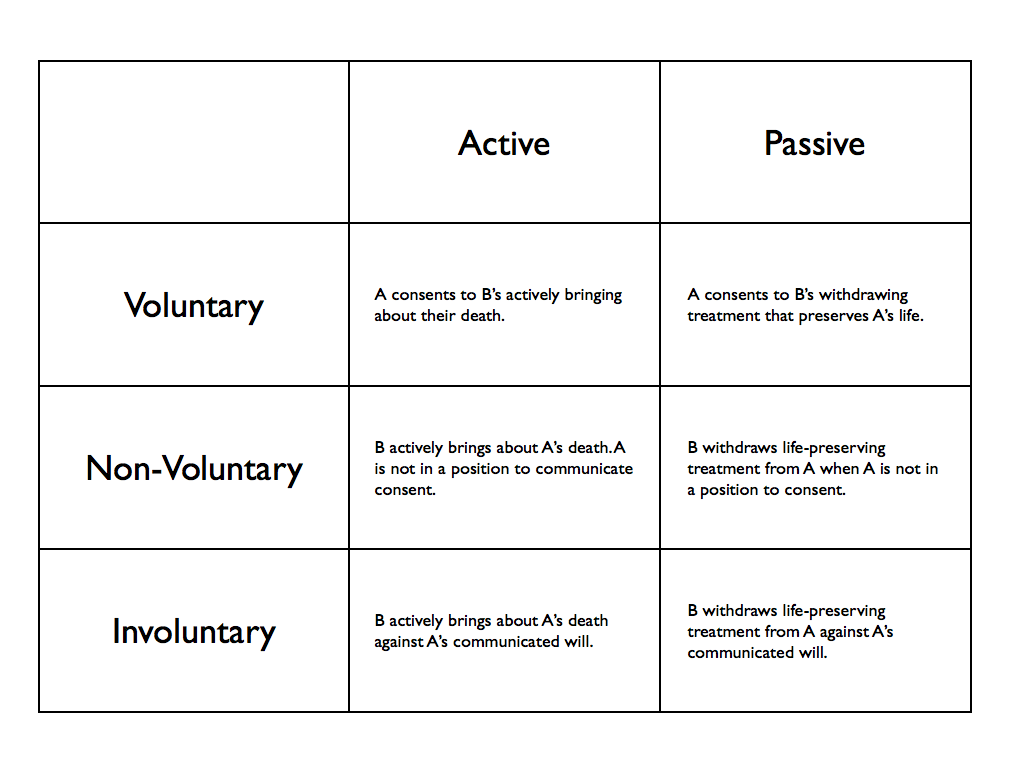
Contemporary Debates in Bioethics presents two perspectives: “Physician-Assisted Suicide is Ethical,” and “Physician-Assisted Suicide is Not Ethical.” It is important to understand that we do not always have to take all measures possible to preserve someone’s life, our own included. It can be morally right to forgo life-sustaining treatment, foreseeing that this will result in dying more quickly than one otherwise would. There is a crucial distinction between intentionally killing and choosing to forgo treatment, foreseeing (but not intending) the death or hastening of death, that will occur as a side effect. Sometimes not doing something can be chosen as a means of bringing about some end. So, it is possible to choose an omission as a way of bringing about someone’s death. In choosing to assist Sue with suicide, the physician diminished his respect for the intrinsic good of human life (Lee 215).
Hence, I agree with Patrick Lee in arguing that physician-assisted suicide is not ethical. It would have been acceptable for the physician to withhold treatment and allow Sue to die (passive euthanasia), but that it was not acceptable for him to assist her in committing suicide (active euthanasia).
In the Media Today / Discussion
This case brought to mind two films that many may have seen: You’re Not You and Me Before You.
You’re Not You is a drama centered on a classical pianist named Kate who, like Sue, has been diagnosed with ALS. When Kate is in the advanced stages of ALS, she is shown sitting upright in her wheelchair and speaking in a labored fashion. The film is valuable in showing the way in which patients in this condition are unable to sit upright because the muscles in their backs are no longer receiving signals from the brain; the same is true of the muscles in the throat and jaw, making speech impossible. Kate says, “I’m going to die. I don’t want to be here.” Do you think that if misery is placing an undue burden on her existence, she may ask for assistance in ending her life? Trailer:
In Me Before You, the lead character is disabled (paralyzed) and chooses to end his life, leaving the newfound love of his life instructions to “live boldly” and encouraging her to live well. I feel that this romanticizes a death wish and promotes suicide as an act of love. What message do you think this sends, and how does his predicament relate to Sue’s case? Should medical aid in dying be considered differently for people with disabilities (Will) than people with terminal illnesses (Sue)? Trailer:
Works Cited
Beauchamp, Tom L., and James F. Childress. Principles of Biomedical Ethics. New York: Oxford UP, 2013. Print.
Lachs, John. “Physician-Assisted Suicide is Ethical.” Contemporary Debates in Bioethics. Chichester, West Sussex: John Wiley & Sons, Inc., 2014. Print.
Lee, Patrick. “Physician-Assisted Suicide is Not Ethical.” Contemporary Debates in Bioethics. Chichester, West Sussex: John Wiley & Sons, Inc., 2014. Print.
Thomas, John E., Wilfrid J. Waluchow, and Elisabeth Gedge. “Case 6.2: Sue Rodriguez: ‘Please Help Me to Die.'” Well and good: a case study approach to health care ethics. Peterborough, Ontario: Broadview Press, 2014. Print.
Hi Elizabeth! I really enjoyed reading your post. It’s tricky to compare the moral implications of passive versus active euthanasia, or in this case, physician-assisted suicide. I specifically want to comment on your questions about how the film, Me Before You, relates to this case. After I watched the film, I viewed Will’s act as selfish. Sure, he was paralyzed; but couldn’t he live with Lou, who loved him dearly, and lead a happy life? Will’s desire to commit suicide came not from fear of the paralysis itself, but of the fear of missing out on his old life. Because he could no longer participate in activities he loved, he felt as if his own identity was taken away. In his eyes, his quality of life, even with a wonderful and supportive girlfriend, was so low that life was no longer worth living.
Unlike Will’s paralysis, which is localized below the neck, Sue’s chronic diagnosis with ALS can do much more damage in the long term. ALS, unlike paralysis, is characterized by muscle deterioration, twitching, and stiffness. Along with altering one’s range of motion, ALS can also make it hard to speak, swallow, and even breathe. Being a chronic condition with no known cure, Sue is guaranteed to die from the illness if something else does not kill her first. Will, on the other hand, is not in any mortal danger due to his paralysis.
After understanding these differences, it is better justified for Sue to commit physician-assisted suicide compared to Will, as his paralysis will not be the direct cause of his death. However, in this case, I think other options besides physician-assisted suicide should be explored for Sue first. As she is in the early stages, perhaps she could enter a palliative care facility so that she can die passively rather than actively. While patient autonomy is important, it must be morally challenging for a doctor to kill his patient as it goes against the principle of nonmaleficence. However, if Sue, a competent individual, continues to express her desire to die even after these alternatives are explored, I think it is morally justifiable to assist her in death. As Dr. Donald Low, diagnosed with a brain tumor, states in his plea to change assisted suicide laws: “Live in my body for 24 hours … I’m just frustrated not being able to have control of my own life, not being able to make decision for myself when enough is enough.” Giving Sue, whose illness controls her, the power to decide how and when to end her life is empowering. While we may think of it as harm, perhaps it helps.
REFERENCES
Kotha, S.R. (2015). What is the difference between ALS and paralysis? Quora. https://www.quora.com/What-is-the-difference-between-ALS-and-paralysis
City Desk. (2013). ‘Who owns my life?’: Sue Rodriguez changed how we think. Windsor Star. http://windsorstar.com/life/who-owns-my-life-sue-rodriguez-changed-how-we-think