Terrence F. Ackerman argues that medical doctors have the responsibility to intervene in their patient’s decision-making if it is in their best interest. The reasoning behind his argument is that illness inherently diminishes the value of autonomy because people who are sick are not competent enough to make their own decisions. This may be due to physical, psychological, or social constraints, relating to their illness or medical situation, which influence their decisional capacity. “Decisional capacity is based on the patient’s ability to understand the choices, to deliberate about those choices, and to articulate his choice. Decisional capacity is dynamic—that is, a patient who had appropriate decisional capacity yesterday may not have it today.” (Marco) I agree with his argument in the sense that doctors should evaluate whether a patient is mentally sound enough to make competent decisions. However, if a patient is mentally sound, a doctor should not override their decision based on a notion of diminished autonomy. There will always be stressors affecting a patient’s decision-making capacity. However, if the patient is not psychologically impaired, they should be able to have final say in their medical treatment, regardless of their physician’s opinion.
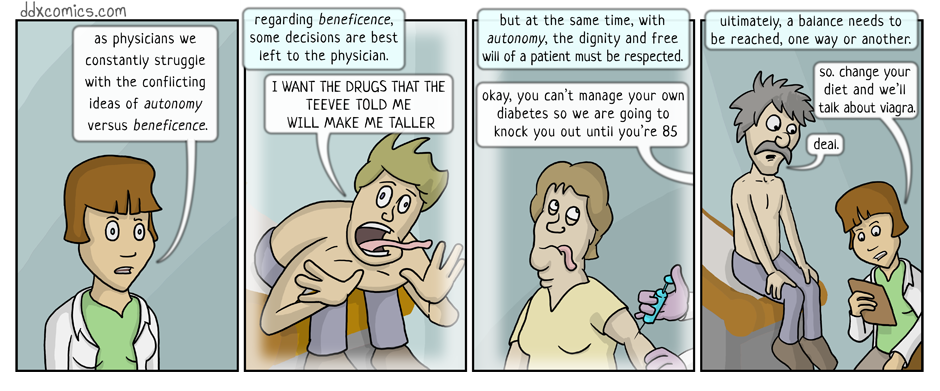
The issue at hand is one of patient autonomy versus the principle of beneficence, in the sense of paternalism. Doctors must weigh whether their duty to help their patient is greater than the patient’s right to make autonomous decisions. Initially, this seemed like a simple decision. A doctor should always ensure their patient is making decisions that are in their best interest. However, the main deterrent to this is that sometimes patients do not agree with their physicians about what course of action is in their “best interest”. Should a medical professional be able to override a patient’s bad medical decision based on their knowledge of the patient’s best interest?
This idea reminds me of the issues we discussed in the beginning of the semester. For instance, Jehovah’s witnesses are forbidden by their religion to receive blood transfusions, even in times of immediate need. When treating a patient who is a Jehovah’s witness, would it be acceptable for a physician to override the patient’s decision to refuse a blood transfusion if it would save the patient’s life? Many would argue that the answer is no, due to the principle of autonomy.
In the end, I believe doctors must come to terms with allowing patients to make decisions that may not necessarily result in their best interest. This does not mean a physician is not entitled to express their professional opinion. In fact, I think the best course of action for a physician is to explain their reasoning to the patient and allow them to make their own decision. “In cases where the choice made will clearly adversely affect the patient, practitioners need not be so neutral that they cannot indicate what they consider to be the best choice. No effort at persuasion is tantamount to abandonment.” (Dunbar) Therefore, doctors should only intervene in patient decision-making by persuading the patient to proceed in one direction versus another. Patients have the right to refuse treatment, even if it is not the best course of action in the eyes of medical professionals. I believe the following quote by Dr. Steven Pantilat appropriately summarizes a physician’s obligations:
“a patient who has had bypass surgery may want to continue to smoke or a patient with pneumonia may refuse antibiotics. In these situations the autonomous choice of the patient conflicts with the physician’s duty of beneficence and following each ethical principle would lead to different actions. As long as the patient meets the criteria for making an autonomous choice (the patient understands the decision at hand and is not basing the decision on delusional ideas), then the physician should respect the patient’s decisions even while trying to convince the patient otherwise.” (Pantilat)
References
Ackerman, Terrence F. “Why Doctors Should Intervene.” The Hastings Center Report 12.4 (1982): 14-17. JSTOR. Web. 18 Mar. 2017.
Dunbar, Terri. “Autonomy versus Beneficence: An Ethical Dilemma.” Primary Health Care. N.p., Feb. 2003. Web. 18 Mar. 2017.
Marco, Catherine A. “Does Patient Autonomy Outweigh Duty to Treat?” Virtual Mentor. Amer Med Assoc, 24 Mar. 2009. Web. 18 Mar. 2017.
Pantilat, Steven. “Autonomy vs. Beneficence.” Autonomy vs. Beneficence. UCSF School of Medicine, 2008. Web. 18 Mar. 2017.
Hi Gisell,
I agree with your conclusion that “doctors must come to terms with allowing patients to make decisions that may not necessarily result in their best interest”. I believe that when a patient is deemed competent, their autonomy should be respected in every situation, even if that means allowing autonomy to override beneficence.
Your blog post reminded me of the discussion that we had in class on Friday about Dax’s case. Dax’s opinion about what was in his best interest drastically conflicted with what the physicians believed to be in his best interest. During Dax’s time in the hospital he believed that death would be the best option for him as opposed to suffering through several procedures and living with the consequences of the incident. However, the physicians believed Dax’s best interest consisted of doing everything they could to save him. In my opinion, Dax’s opinion should have been respected in this situation. I think it was a violation of human rights for the hospital to have treated Dax the way they did.
Ryan Blum brings up an interesting counter argument when he asks if the conflict between autonomy and beneficence would change if “the situation is… one in which the patient’s decisions may have a substantial impact upon the life of another who is dependent upon the patient for support” (Blum). This argument could be applied to Dax’s case if we took into consideration his family. However, I still believe that in the end, whether or not his family depends on him, Dax’s autonomy overrides any counter argument. One can assume that in making his decision, Dax would likely take into consideration how his family would be impacted. As a result, I remain firm in my position that the patient’s autonomy should override the principle of beneficence when the patient is deemed competent.
Morgan Brandewie
Works Cited:
Blum, Ryan. “When Patient and Physician Disagree on Patients Best Interest.” Virtual Mentor. Amer Med Assoc, 18 Aug. 2010. Web. 19 Mar. 2017.
Hi Gisell!
I think you bring up some really great points in your blog post. First, I too agree that as long as the patient is not psychologically impaired, they should be able to make the final decisions regarding their treatment and course of action even if it conflicts with the physician’s recommendation. In Ackerman’s article, he references Edmund Pellegrino who claimed that when a patient is ill, he or she “lacks the knowledge and skills necessary to cure himself or gain relief of pain and suffering… The state of being ill is therefore a state of ‘wounded humanity,’ of a person compromised in his fundamental capacity to deal with his vulnerability” (Ackerman 15). I take a lot of issue with this claim because not everyone who suffers from an illness is incompetent, and if a patient is not deemed incompetent, they should be able to make their own decisions. The patient may not have the “knowledge and skills necessary to cure himself” in terms of medical school or extensive amounts of outside medical knowledge; however the patient has the knowledge of his or her own moral values and obligations. Combining the moral values and obligations of the patient with the medical knowledge on behalf of the physician is enough information for any competent patient to make their own decision that should be respected by the physician.
As we have been talking about in class, I don’t think it is necessary or ethical for the physician to simply take the patient’s decision at face value if it appears to be unconventional or surprising. In order to make sure the patient is drawing their conclusion from accurate information, I think engaging with the patient and probing their reasoning is a great way for the physician to understand where the patient is coming from and ensure that the decision of the patient is in what the patient believes to be his or her own best interests. It is possible for the physician and patient to have different opinions on what is in the patient’s best interests; however at the end of the day, if the patient is deemed to be competent, the patient’s view of his or her own best interest should trump the physician’s opinion. As autonomous beings, we should have the right to make our own decisions; not all of them will be great decisions or ultimately be in our best interests, but I think, as long as it does not cause harm to others, it is our right as individuals to be able to make that choice.
References
Ackerman, Terrence F. “Why Doctors Should Intervene.” The Hastings Center Report 12.4 (1982): 14-17. JSTOR. Web. 18 Mar. 2017.
Hi Gisell,
I appreciate your reflection on the blood transfusion case that we analyzed at the beginning of the semester; this was a very thoughtful application of the relationship between patient autonomy and the principle of beneficence.
The principle of beneficence has seemed to many to constitute the very soul of morality. It demands that we actively promote the well-being of others and prevent or remove harm to them. Accordingly, there is little doubt that the health care professionals have such a duty to their patients, as advancing their welfare, promoting their well-being, and preventing or removing harm to them are large parts of what they are obliged to do (Vaughn 10).
Hence, I agree with Terrence F. Ackerman that physicians and other health care professionals have a moral obligation to intervene in the decision-making of an incompetent patient. Like Morgan and Gabby, I argue that competent patients, however, have the right to refuse treatment, even if it is not the best course of action in the eyes of the physician.
Dependence on Competence:
By inference, a greater weight must therefore be placed on patient autonomy if the patient is competent; if the patient is incompetent, a greater weight must be placed on the principles of beneficence and utility and thus the moral obligation of the health care professionals to promote the well-being of the patient.
Works Cited
Vaughn, Lewis. Bioethics: Principles, Issues, and Cases. New York: Oxford University Press, 2010. Print.
Perhaps the most important aspect of autonomy is that it gives patients the right to make “stupid” decisions. While deleterious to their health, there is something valuable in having respect for a patient’s unintruded self-determination. As long a the physician acts in the interest of the patient and does their best to promote productive, healthy choices, the patient should retain full autonomy and be the final decision maker (assuming they are mentally competent to make the decision). It’s not so much about the patient making a specific good decision, but rather about the patient having the opportunity to act of their own accord.
Since autonomy usually isn’t discussed outside the context of controversial decision, it generally stands in opposition to beneficence. The ethical dilemma comes down to balancing these two principles, with autonomy representing the patient’s freedom and independence, while beneficence represents paternalistic physician control. I agree that physicians should be allowed to challenge their patients and continue to give their input/advice when they suspect the patient of not acting in their own self interest. Yet this is persuasion on behalf of the physician, not actual control over the patient. While this can certainly present a notable impact on what the patient ultimately decides to do, it preserves autonomy and attempts to maximize beneficence, which is what I view to be one of the most crucial roles for a physician.