Background
There are many ethical problems posed in the case regarding Henrietta Lacks. Unfortunately, her case occurred during a time where black individuals did not have the same rights as white individuals. This discrimination lead to black patients being treated only under the condition that it was then appropriate for medical research to be conducted on them. The two ethical issues I will tackle in this blog are should patients give consent to having their cells researched? Furthermore, to what extent should we violate autonomy to advance science?
Dilemma
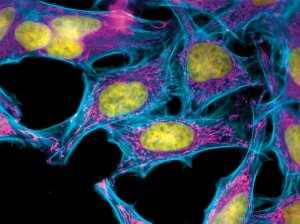
Lack’s cells were special as they were the first successfully grown human cells. Her cells led to many advances in the scientific community such as leading to the eradication of polio, a disease that plagued many. When Lack’s tumor cells were taken after her death from cervical cancer, “no one asked her permission to take the cells” (p. 254). However, the case did state “it was considered fair for medical researchers to conduct research on patients because they were being treated free of charge” (p. 254). Operating under this principle, which I believe violates autonomy of black individuals, I will evaluate whether the principle of autonomy was violating regarding Lack’s cell collection. It is clear that the racism at the time was unethical for a multitude of reasons and the case does not make it clear whether Lacks was aware that by receiving medical attention free of charge she was giving herself to research. If she was unaware of the extent to which research would occur on her, than this would violate the principle of autonomy because she did not give consent to the researchers. I believe that it is easy to agree that patients should consent to any research that might be conducted on them as without consent autonomy is violated.
However, if upon entering the hospital Lacks was informed that they would treat her only under the circumstance that her cells would be used for research later, than I do not believe her autonomy was violated past the violation of autonomy as a result of racism. Beauchamp and Childress state, “nothing about economically disadvantaged persons justifies their exclusion, as a group, from participation in research, just as it does not follow from their status as disadvantaged that they should be excluded from any legal activity” (p. 268). Since Lacks was financially disadvantaged, one could argue that she is being exploited by receiving medical attention from this hospital. However, if one were to continue down this path then in an attempt to “eliminate the problem of unjust exploitation” society would have to “deprive these individuals of the freedom to chose [to engage in research]” which “would often be harmful to their financial interests” (p. 268).
Reflection
One of the conditions of the principle of justice is allocation of resources. Allocation of resources implies that if “there is not enough to go around, [then] some fair means of allocating scarce resources must be determined” (principle of bioethics online website). What if we could make the resource less scarce? Then issues surrounding justice and prioritizing distribution would be less of a concern. In Lack’s case researchers utilized her cells after her death, and advanced science exponentially as her cells were the first “ever successfully grown human cells in a lab” (p. 254). In regard to organs, after individuals are deceased and are not organ donors, their organs decay, providing no advancements or cures for live individuals suffering medical conditions. Does it seem logical to allow all the organs or people who are not organ donors to go to waste after death? Should we as a society utilize the bodies of not only donors, but also individuals who are not labeled donors after their death for the advancement of science? Many would argue strongly against this, expressing concern that this blatantly violates the person’s autonomy and free will. However, currently arguable greater ethical violations are occurring due to the lack of available organs. Individuals might contemplate having another child for the primary purpose of providing one of their current children an organ necessary to live. Is this a greater violation of autonomy than taking the organs of someone who has lived a full life and now has died? The person who is dead would be unaware their autonomy is being violated unlike the child who will later realize that their autonomy was violated from a young age. In Lack’s case, her cells were taken after her death. Looking back, knowing all the amazing advancements that occurred as a result of her cells, it is difficult to imagine where we would be today without her cells. Nobel prizes, the treatment of polio, and cell culture industries all resulted from Lack’s cells. It is fascinating to imagine the advancement that could result from having access to organs after individuals are deceased. An average of 21 people die a day waiting for an organ transplant (http://www.organdonor.gov/about/data.html), it is interesting to think about how many lives we could save by implementing a policy regarding organ donation of the deceased. Furthermore, if we had an ample supply of organs, researchers would have more material to investigate and try treatments on, which could lead to eradications of other diseases and conditions. Although this notion seems far fetched, I think it is an interesting idea to consider in the light of Lack’s case. While Lacks was alive she was provided with medical attention and treatment she would not have received without the possibility of research on her cells after her death. If Lacks gave consent to the researchers allowing them to conduct research on her after her death, even though there is the concern of exploitation, I do not feel it was wrong to utilize her cell’s after her death. The main moral issue I found with this case was the lack of acknowledgement and compensation her family received after the success of her cells. The case states, “Henrietta’s family remain[ed] in poverty and have never received any benefit or recognition for their mother or grandmother’s contribution to science” (p. 254).
Work Cited
“African American Trailblazers in Virginia History.” N.p., n.d. Web.
Thomas, John E., Wilfrid J. Waluchow, and Elisabeth Gedge. “Case 7.3: Who Owns the Research? The Case of the HeLa Cells.” Well and Good: A Case Study Approach to Health Care Ethics. 4th ed. N.p.: n.p., n.d. 254-55. Print.
Principles of Bioethics. Thomas R. McCormick, D.Min., Senior Lecturer Emeritus, Dept. Bioethics and Humanities, School of Medicine, University of Washington, n.d. Web. <https://depts.washington.edu/bioethx/tools/princpl.html>.