Background:
Over the past couple of centuries, numerous countries have proposed the implementation of healthcare systems with a socialized approach. The United States of America has had lengthy debates over implementing a socialized medicine program. Currently, citizens of the United States of America have the opportunity to receive either Medicare or Medicaid if requirements for one of the programs are met. “Medicaid provides health coverage to millions of Americans, including eligible low-income adults, children, pregnant women, elderly adults and people with disabilities” (Medicaid.gov). Medicaid is geared toward the lower-income portion of the population that may not be capable of affording private health insurance. “Medicare is the federal health insurance program for people who are 65 or older, certain younger people with disabilities, and people with End-Stage Renal Disease” (Medicare.org). Medicare, on the other hand, is designed to support the health of the elderly portion of the population that may require additional healthcare.
In B.Brody and D. Engelhard’s article, Access to Healthcare, there are three cases presented. Each case depicts an episode in which an individual is in a predicament over healthcare costs and/or accessibility to ample healthcare.
Case A refers to a man who needs surgery at some point in the future. The surgery is not urgent. The problem that the man has is that he cannot afford the surgery, and the company  that he works for does not provide health insurance benefits.
that he works for does not provide health insurance benefits.
Case B refers to a mother whose child is sick. The child needs to see a doctor about a high fever, but the doctor is effectively inaccessible. The journey would be too far and take too long to make it to the doctor.
Case C refers to an elderly couple. T he husband is beginning to show symptoms of Alzheimer’s disease, and is in need of additional nursing care. The couple cannot afford to both keep their house and to send the husband to a nursing home. A lawyer tells the wife that the best financial and legal option is to divorce the husband and claim all assets. Once completed, the husband would comply with Medicaid guidelines.
he husband is beginning to show symptoms of Alzheimer’s disease, and is in need of additional nursing care. The couple cannot afford to both keep their house and to send the husband to a nursing home. A lawyer tells the wife that the best financial and legal option is to divorce the husband and claim all assets. Once completed, the husband would comply with Medicaid guidelines.
Dilemma:
In all three of these cases, shortcomings of America’s current healthcare system are presented. The question to be answered here is “to what extend at what cost ought a society attempt to provide equal healthcare for all?” (B. Brody and T. Engelhard, “Access to Health Care,” Bioethics: Readings and Cases).
Conclusion:
The sanctity of human life plays a major role in this dilemma. Is it morally just to not provide a portion of the population with accessible and high-quality healthcare? In my opinion, everyone is entitled to healthcare by their basic human rights. If someone does is not provided healthcare, they could die from a simple bacterial disease that in modern times, we can combat with just a few doses of antibiotics. This costs society just a few cents per dose, and yet saves lives. Society cannot justify not providing healthcare for all because if they do not do so, the poorer portion of the population will have no access to healthcare, and pass away from illnesses in which we have proven cures. Society is harming individuals that do not have healthcare.
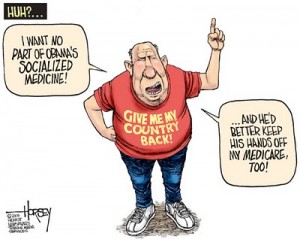
Recently, America is moving towards healthcare reform in which a socialized medical approach will be instituted. President Obama has established the Affordable Care Act in order to help expand coverage, lower healthcare costs, and enhance the quality of care for participants. The implementation of this Act allows anyone who desires health coverage to acquire health coverage.
With this recent implementation of healthcare reform, all three cases will be resolved. In case A, the man can now afford to purchase a subsidized healthcare plan in order to afford surgery. In case B, the mother should be able to see a closer doctor because she no longer needs to go and visit a charity doctor. In case C, the health insurance prices could be lowered so that they are affordable for the elderly couple. Just like with any legal reform, there are individuals that are left out of the benefits. While this does not solve the problem of inaccessible healthcare for the entire population, this reform does benefit a significant number of individuals and is a step in the right direction for the morality of the United States healthcare system.
In conclusion, as a society, we have an obligation to ensure the health of our entire population. The sanctity of life is paramount. No matter the cost, society ought to attempt to provide equal healthcare for all.
Works Cited:
http://medicaid.gov/affordablecareact/affordable-care-act.html
https://www.medicare.gov/
B. Brody and T. Engelhard, “Access to Health Care,” Bioethics: Readings and Cases
http://goodtoknow.media.ipcdigital.co.uk/111/000000d5c/b9e6_orh220w334/elderly-couple-dementia-relationship-grandparents.jpg
https://dss.sd.gov/img/behavioralhealth/motherson.jpg
https://waxingtofull.files.wordpress.com/2012/01/horsey-healthcare-socialized-medicine1.jpg


 Placebos are inert and don’t cause anything (Moerman DE, Jonas WB).” This statement may not be entirely valid, but the point is that placebos are not as effective as the correct treatment. “I don’t believe that the use of placebos is immoral or unethical. In reality, it seems that the medical profession’s lack of understanding and utilization of the mechanism of the placebo in the healing process is tragic, shortsighted and cowardly (wrf.org).” It may be easier for physicians to approach placebos and say that they do not work, but evidence proves that if used, placebos do work between 30%-60% of the time (wrf.org). As long as a patient is receiving the most beneficial treatments prior to administration of placebos, doctors ought to utilize placebos when no other viable treatment is present.
Placebos are inert and don’t cause anything (Moerman DE, Jonas WB).” This statement may not be entirely valid, but the point is that placebos are not as effective as the correct treatment. “I don’t believe that the use of placebos is immoral or unethical. In reality, it seems that the medical profession’s lack of understanding and utilization of the mechanism of the placebo in the healing process is tragic, shortsighted and cowardly (wrf.org).” It may be easier for physicians to approach placebos and say that they do not work, but evidence proves that if used, placebos do work between 30%-60% of the time (wrf.org). As long as a patient is receiving the most beneficial treatments prior to administration of placebos, doctors ought to utilize placebos when no other viable treatment is present.

