VA Whole Health Model and Chaplaincy Focusing on What Matters Most to the Veteran
Introduction
For the past four years I serve as a board-certified clinical chaplain with a specialty in post-traumatic stress disorder (PTSD) at Bay Pines Veterans Affairs Healthcare System (BPVAHCS). I provide ministry to a diverse veteran population alongside eight chaplains from different faith traditions.
During this project, I transitioned from the acute care chaplain to the position of mental health chaplain for the medical facility. This change in assignment, drastically altered my scope of practice and customer base. I intentionally developed excellent relationships with mental health professionals, read books such as the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)[i], and journal articles to learn the language of the mental health field.
A qualitative study was performed focusing on the Veterans Affairs (VA) new spirituality process (spirit and soul) of the Integrated Whole Health Patient Care Model and how it influences the spirituality of the veterans/patients on the medical/surgical unit 5B at the Bay Pines Veterans Healthcare System (BPVAHCS). The new process of using the whole health spiritual care model (spirit/soul) in its current state will change the trajectory in which spiritual care is offered to veterans/patients. As a result, discovering how veterans’ faith impacts their healing process is vital to know if the whole health model is useful in helping veterans.
The Department of Veterans Affairs senior-level executives have decided to undergo a paradigm shift from a medical model of patient care to a whole health model of patient care. The medical model of care is the traditional approach to the diagnosis and treatment of illness as practiced by physicians in the western world. The physician focuses on the defect, or dysfunction, within the patient, using a problem-solving approach. The medical history, physical examination, and diagnostic tests provide the basis for the identification and treatment of an illness. The medical model centers on the physical and biological aspects of specific diseases and conditions.[ii]
The whole health model integrates the veteran’s values and those things that are significant to the veteran into a plan of care. The whole health model includes a series of eight fundamentals which are 1) Working your body: Moving the body can take many forms such a dancing, walking, gardening, yoga, and exercise. 2) Surroundings: One’s surroundings at work and where one lives can affect one’s health and outlook on life. 3) Personal Development: One’s health is impacted by how we choose to spend our time. Aligning activities with what matters to us can help in the healing process. 4) Food and Drink: The veteran’s nutritional intake can influence health physically and mentally. 5) Recharge: Getting enough rest, relaxation, and sleep is vital. 6) Family, Friends, and Coworkers: Connecting to people who care about the veteran is helpful to the healing process. 7) Spirit and Soul: Having a sense of purpose and meaning in life, finding strength is useful to the healing process. 8) Power of the Mind: Connecting with the power of one’s mind to heal and cope.
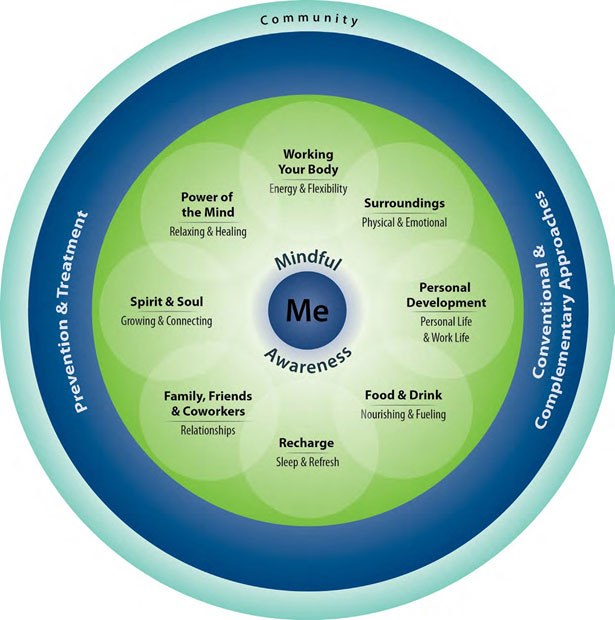
Diagram 1: Whole Health Model[iii]
These eight components collectively represent whole health self-care, which includes all the decisions one makes daily that affect physical, mental, and spiritual health. Within these eight practices is the practice of mindful awareness, which means being fully aware, or paying attention now so that one can make conscious, proactive choices about every aspect of their health. Another area is an element that serves the professional care received as a part of the prevention and treatment of illnesses or diseases, including both traditional and complementary medicine, such as acupuncture, yoga, tai chi, and mind-body therapies. Lastly is exploring the community the patient connects to and the influence in their life.[iv]
Veterans Affairs Clinical Chaplains are the designated subject matter experts for spiritual and pastoral care for patients, and the management of chapel facilities.[v] Chaplains bring a unique perspective to the multidisciplinary healthcare team; the chaplain, through God’s revelation, reveals to the group how the patient’s spirituality or nonexistence of spirituality is influencing their healing/recovery process. It is the clinical chaplain’s responsibility to ensure that every patient’s constitutional right to free exercise of and protection from proselytizing.
The hospital chaplain walks between two worlds: religion and medicine, though a member of the medical community, they do not admit, diagnose, medicate, or discharge patients.
They embrace inevitable change, critically examining faith modalities, and providing exceptional patient-centered pastoral care.[vi] Communicating why change is necessary is helpful in gaining veterans and stakeholders’ support. When they elect not to participate in change, it creates a vacuum that other clinicians, such as social workers or mental health professionals, fill the space.
Resulting in an approach leading to veterans’ spiritual choices being curtailed. Clinical chaplains are spiritual, and culture navigators trusted troubleshooters revealing to the multidisciplinary team how the veteran’s faith and culture are influencing their healing process. They are invited into the sacred space of veterans’ life experiences. They listen to the language of the soul and function as the divine trust factor, ensuring that veterans’ spirit and soul whole health choices are honored[vii].
Learnings from the Project
Within the Veterans Affairs Healthcare System, there’s an overabundance of obstacles to performing tasks. There is the issue of a patient’s privacy, along with many rules and regulations that must be meticulously followed, and often sections work independently and unwillingly to collaborate with others. It is to engage in an enormous medical system that is continuously evolving with ambiguities, complications, and blurred realities.[viii]
A qualitative approach was employed to gather and analyze pertinent data by conducting oral feedback interviews. Ten participants on medical/surgical unit 5B were identified and invited to participate in the study based on the last digit of their social security number ending in number two. They were asked questions about their impact of military service, approach to their spirituality in a medical setting, meaning in life, definitions and practices, sources of peace, community, and understanding of spiritual practices.
Barriers to Whole Health were high in our veteran sample. The research revealed that Bay Pines serves the oldest veteran population within the VA medical system. Age was significantly related, indicating that older veterans are having more difficulty connecting to the whole health spirituality model. These older veterans are comfortable with their religious traditions. They are fearful of using technology, which indicates that older veterans may need assistance to access the Whole Health model of care. Veterans suffering from combat-related illnesses such as TBI, PTSD, pain, depression, substance use, and elevated suicide risk represent a unique and high-risk population.[ix]
Whole Health directly addresses these problems through the eight components of well-being, which include: working your body, surroundings, personal development, food and drink, recharge, relationships, spirit and soul, and power of the mind. Whole Health is a nationwide change that all VAs will be expected to adopt. Implementation of the Whole Health model of care needs to be the complete adoption of a new culture in the Residential Medical/Surgical Treatment Unit 5B at the Bay Pines VA Health Care System. The values of Whole Health originate from empowering veterans to act in their healthcare through prevention and well-being.
Investigating veterans’ health philosophy at their entry point to VHA can help the veteran to determine if the veteran could benefit from a more integrative approach through the offering of a comprehensive treatment plan inclusive of the Whole Health model of care. With the availability of the Whole Health model of care, current and future veterans can take advantage of a nonpharmacological treatment plan with wellness goals designed to stop the progression of the disease.
[i] American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, American Psychiatric Association, 2013.
[ii] U.S. Department of Veterans Affairs. “The Whole Health System” accessed June 17, 2018. Https: www.va.gov/patientcenteredcare. 17.
[iii] https://www.va.gov/WHOLEHEALTH/circle-of-health/index.asp
[iv] Paul J. Mills, “Advancing Research on Traditional Whole Systems Medicine Approaches,” Sage Journals 22, no. 4 (October 2017): 527-530, accessed June 24, 2018, https://doi.org110.117/2156587217745408.
[v] Veterans’ Health Administration Directive 1111(1). Spiritual and Pastoral Care in the Veterans Health Administration. Washington DC. 2016. 7.
[vi] Leah D. Bueckert and Daniel S. Schipani. Editors, Spiritual Caregiving in the Hospital Windows to Chaplaincy Ministry. Pandora Press Publishing, Kitchener, Ontario. 2006. 1.
[vii] Martin L. Smith. Chaplaincy and Clinical Ethics: A Common Set of Questions. Hastings Center Report 38, no. 6. 2008: 28-29.
[viii] Lawrence E. Holst, ed. Hospital Ministry the Role of the Chaplain Today (New York: Crossroad Publishing Company. 1985), 3.
[ix] Steve Bloem, The Pastoral Handbook of Mental Illness A Guide for Training and Reference. (Grand Rapids: Kregel Publications Publishing, 2018), 138.