After taking this class and traveling to Guatemala to work with community health workers, I realize how important and influential community mobilization is toward a necessary change. I found a really great guide published by USAID that details how communities can be mobilized specifically toward improved maternal and newborn health. It details the problems that mothers and unborn children face at birth, all of which we’ve outlined throughout the semester (i.e.-the three delays). It talks about common complications, potential illnesses, and their appropriate interventions. Yet it also highlights the importance of including the community as drivers for change and the ways in which this can be accomplished. The document explains this necessity:
“Any approach to improve essential maternal and newborn care services must address the issues of the community and the health system together, systematically, and in close collaboration among all stakeholders if it is to be successful.”
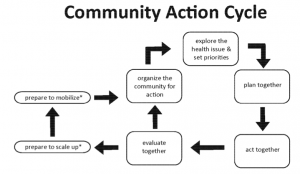
It includes the use of the “Community Action Cycle” as pictured above. This involves different phases such as organization of community stake-holders, planning outcomes and interventions, and preparing to mobilize. However, the cycle doesn’t start or end at a designated point because all communities operate differently. The important part of community mobilization is identifying appropriate stakeholders (mothers, health workers, community leaders, government leaders, etc) and having them establish strategies for issues that the entire community is affected by. Finally, in order for change to be sustainable, mobilization has to continue and consistently be reinforced within the community. I think this is a great tool to use for individuals or groups who are considering using this method whether it be for infant and maternal health or for any other public health issue.
USAID & ACCESS. (2009). How to Mobilize Communities for Improved Maternal and Newborn Health. Retrieved from http://www.accesstohealth.org/toolres/pdfs/access_cmmnh.pdf