I’ll Be There for You
by Kiara Mehta
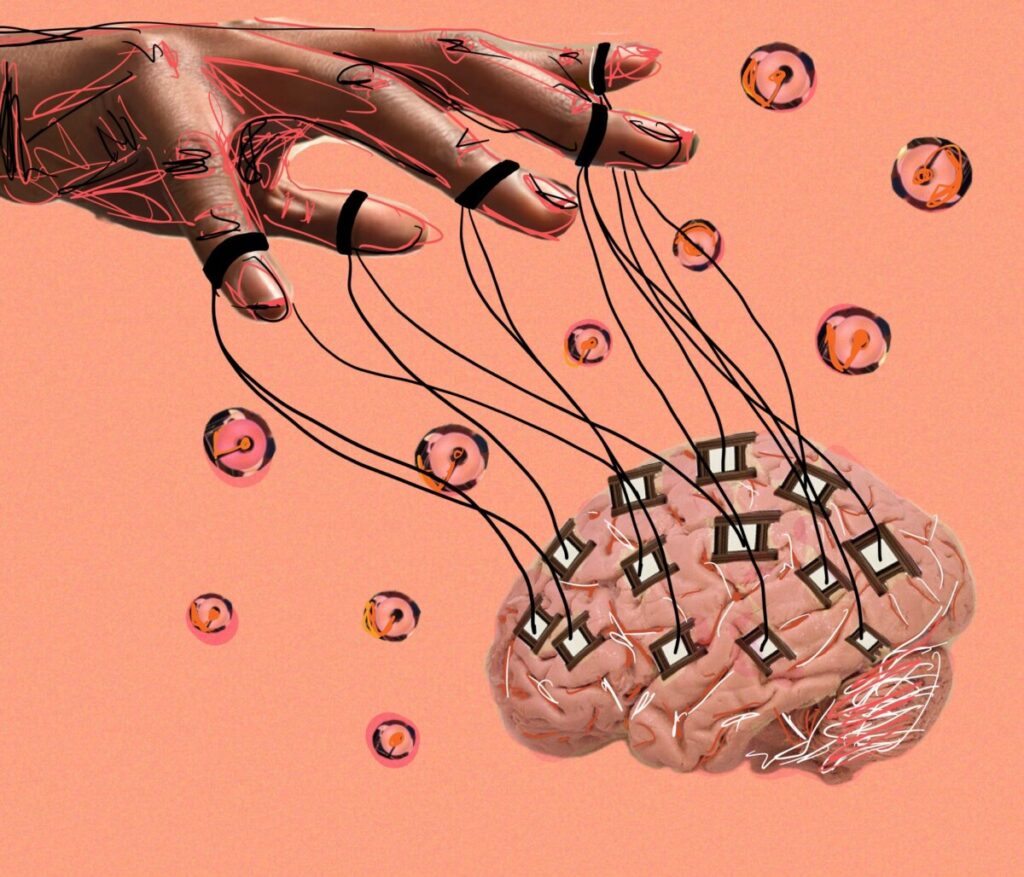
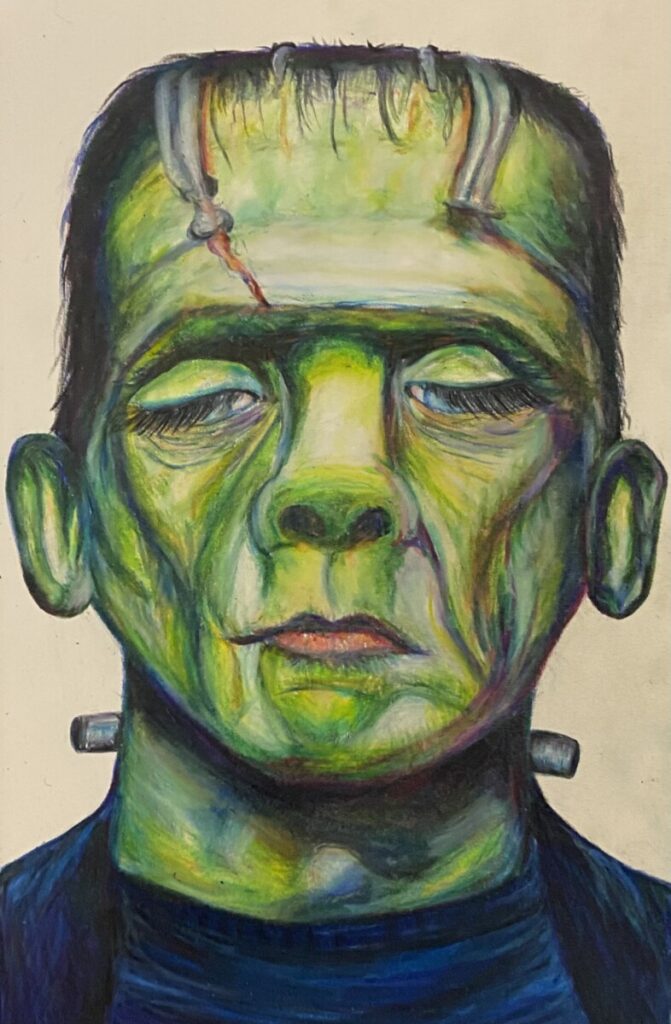
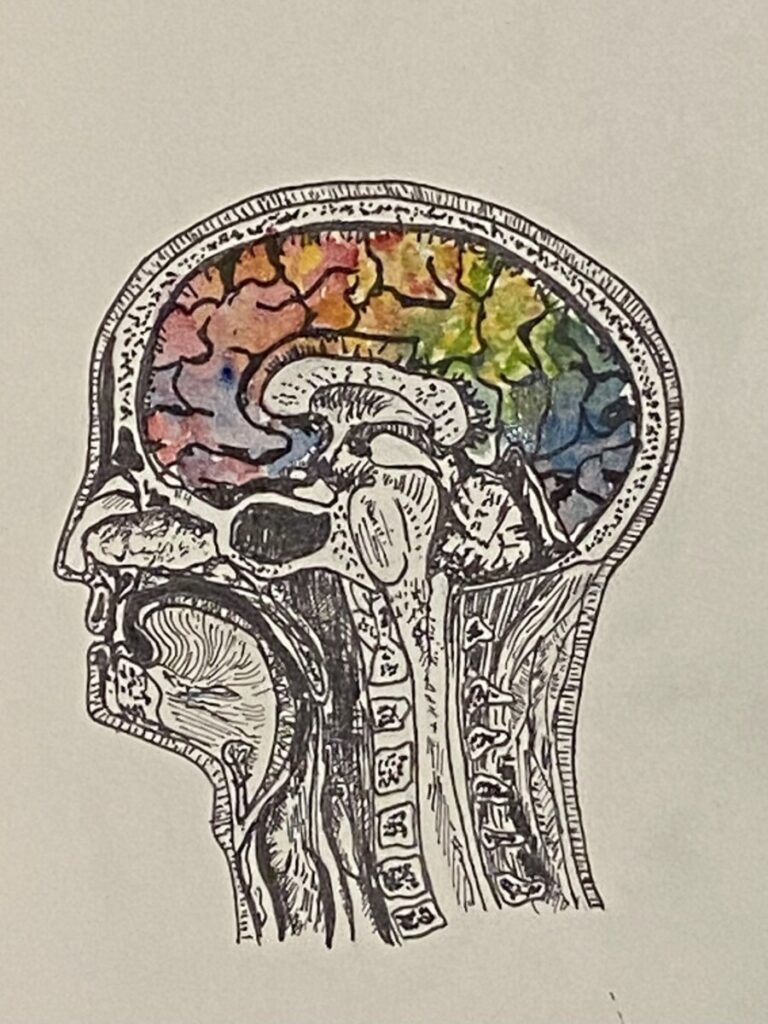
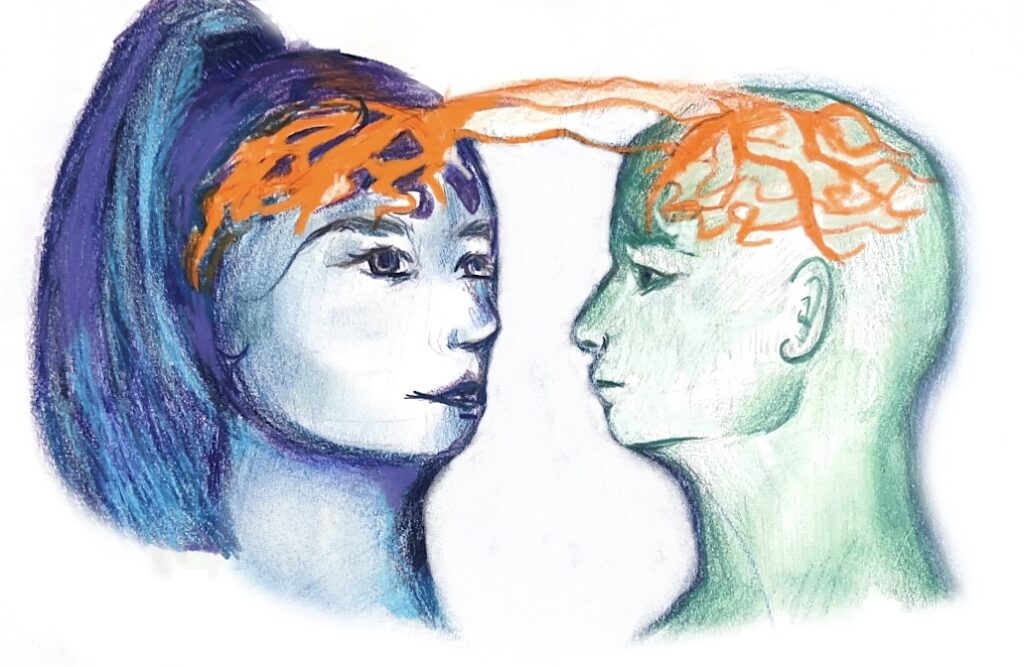
art by Laura Zang
Who is your best friend? Perhaps it is someone you met years ago from your hometown or simply someone you met this year in school, at your job, or enjoying a hobby. Think about how you established a friendship with this person and how much they impact your life. Did your relationship come naturally? Does it feel as though your friend makes up an essential part of who you are? Can you imagine your life without this person? While these questions might not be the first that come to mind when you think of your best friend, they are the basis of what allows us to understand why we chose to be friends with certain individuals and how they impact who we are. Making friends and establishing relationships is a fundamental human behavior affected by multiple factors, including culture, age, interests, etc. The human brain, among these, resides as an equal, if not more influential, part of who we seek to call our friends. The human brain plays a part in not only who we choose to establish friendships with, but how our friends shape, influence, and change our brains.
Who Do Humans Consider Friends?
From the people we see on a daily basis, to those who we confide in with our thoughts and typical worries, it can be challenging to pinpoint what a friend is. That is why there is no exact definition for a friend, as it varies individually. However, Lauren Brent, a neurobiology professor at Duke University, defines ‘friends’ as “pairs of individuals that engage in bi-directional affiliative (nonaggressive, nonreproductive) [nonsexual] interactions with such frequency and consistency so as to differentiate them from nonfriends” [1]. From this, friends seem to be two individuals that chose to continually surround themselves with each other on a regular basis. Nevertheless, the subjective nature of friendship needs further examination. For example, are we truly limited to only one friend? What degrees of frequency and consistency are necessary to consider individuals friends—are people who we feel fond of but see twice a year not actually our friends? If nonreproductive behavior is excluded, do other types of friendships such as those of sexual nature count? While the answers to these questions vary from person to person, Christopher Roberts-Griffin, a researcher who studies frequent and desired qualities of friendship, notes that similarity, among other factors, deeply affects what those answers could be [2].
How Does the Human Brain Influence and Decide Who Are Friends?
Have you ever come across someone that you were able to get along with so well despite recently meeting them? If you have, you might have experienced the act of “clicking”. One of the most influential factors that our brain takes into account when deciding who our friends are is our ability to click with certain people. In other words, when the key components of an individual’s personality fit with someone else’s so much so that, over time, establishing a friendship becomes almost natural, these two individuals have clicked. However, the underlying science of how people click stems past face value into the world of complex neural processes and components. Carolyn Parkinson, a psychology professor at the University of California Los Angeles, measured the brain activity in individuals to see how likely they were to become friends based on their response to watching a movie. Parkinson notes, “more generally, people who responded more similarly to the videos shown in the experiment were more likely to be closer to one another in their shared social network, and these effects were significant even when controlling for inter-subject similarities in demographic variables, such as age, gender, nationality, and ethnicity” [3]. Because of this, Parkinson concludes that similar brain activity in parts of the brain like the nucleus accumbens and amygdala makes us click with certain people and thus makes friendships more likely. Our nucleus accumbens plays a major role in our motivation, actions, and reward experiences, while our amygdala is vital for basic emotions by processing our responses to external stimuli [4]. Together, the nucleus accumbens and amygdala influence our everyday actions and emotional responses to others and the environment. Our motivations, goals, and emotional responses play a critical role in today’s society. Perhaps individuals whose brain activity shares similar emotional and motivational characteristics are able to click with one another. This may be due to the weight that our motivations, goals, and emotional responses have in today’s society. Thus, how similar individuals are is a fundamental factor in establishing friendships.
While clicking with certain people is vital to establish formative friendships, first impressions are just as important. Daniela Schiller, a researcher at the Center of Neural Science at New York University, demonstrates that within seconds of meeting someone, the amygdala and posterior cingulate, which plays a role in cognition, form conclusions and quick decisions about people [5]. Not only does the amygdala take on important roles such as processing our environment and emotions, but it also enables us to form quick ideas and make assumptions about people around us. Ultimately, our amygdala considers these ideas to decide if we should continue becoming close friends after initial first impressions.
How Does Brain Activity and Behavior Reflect Those of Friends?
Spending an extensive amount of time around our friends can lead to our brain activity and behavior reflecting theirs. For example, Tanya Chartrand, a professor at Duke University, refers to a concept known as the chameleon effect, where people perform “nonconscious mimicry” of those around them [6]. Across three experiments, Chartrand showed this effect by observing participants in his study who unintentionally matched certain behaviors. In the first experiment, the participants’ motor behaviors inadvertently matched the motor behavior of strangers when working on a task together [6]. In the second experiment, mimicking posture and movement was correlated with interactional flow (smoother interaction). Imitating posture and movement was also positively correlated with likeness among participants. [6]. Finally, the third experiment demonstrated that individuals who were shown to be more empathetic carried out the chameleon effect to a greater extent than others [6]. While there is much more to learn about why and how the human brain unconsciously picks up our friends’ behaviors, Chartrand’s results show that by unintentionally mimicking the actions and behaviors of those around us, even just through simple tasks, we become more fond of them. We then continue to strengthen relationships, which, in turn, increases the frequency of the chameleon effect. This provides valuable insight into how our ability to click with others and cooperate is a way for our friends to influence how we carry out our actions.
It is clear that how we are a reflection of our friends stems from a neurological basis. If our friends affect our physical behaviors, does this mean they are directly affecting our brain’s behaviors too?
Yes, but not in the way you think. Referring back to Parkinson’s research, friends have “exceptionally similar neural responses” compared to individuals who are distant in a social network. Parkinson chose a cohort of friends to watch a collection of video clips that varied in topics and genres to keep familiarity among the participants constant and attention constrained. Despite this, all participants were shown the same video clips in the same order to account for individual differences in the way stimuli were processed. Activity in the hippocampus (which plays a role in memory), putamen (which aids in movement), and amygdala was recorded. FMRIs of the amygdala and putamen showed that friends are very similar to each other in terms of how they “perceive, interpret, and react to the world around them”. Emotionally, we are very similar to our friends on a neurological basis. As a result, we tend to surround ourselves with individuals who not only think but also feel the same way we do. In addition to behaving analogously to our friends, our brain activity shows we are emotionally alike as well. Nevertheless, Parkinson notes further research must be done in order to determine if neural response similarity is a “cause or consequence of friendship” [3].

How Do Friends Change the Human Brain?
The human brain has a predominant role in choosing our friends. But how do our own friends influence and change our brains over time? Brittany Woods, a psychologist at Boston University, notes that close friends positively affect one another’s brain by lowering response in the lateral prefrontal cortex. The lateral prefrontal cortex is believed to deal with affect reappraisal, the process of reevaluating emotionally salient situations to respond and cope differently by decreasing overcontrol of positive emotions, resulting in an overall more positive affect [7]. Woods also noted, “neural response to their own close friend relative to an unfamiliar peer was related to greater activation in a cluster that encompassed both the caudate head and the septum, a region implicated in many affiliative processes such as unconditional trust” [7]. It is important to recognize that while some individuals vary with their amount of trust when initially meeting someone, that over time, they may learn to become more trusting as a result of establishing formative friendships.
Conclusion
Given the research that has been done exploring how our brain influences who our friends are and how our friends affect our brain, it is clear that our brain plays a prominent role in our social life. However, that is not to say that the brain is the sole factor that affects how we make friends. Making friends, as straightforward and natural as it may seem, is the result of a very complex process. Even more so, this process differs from person to person. With these underlying variations, it may be beneficial to research why the process of making friends is so different among people. Furthermore, more research can provide insight into why, neurologically, some individuals have a more difficult time establishing close and lasting friendships compared to others. In any case, it is important to recognize that our friends affect us in different ways and that our brain is a direct reflection of their effect on us as well as our decision to establish friendships with them. So, the next time you are around your best friend, remember your friendship, in part, stemmed from your very own brain.
I’ll Be There for You Read More »