So, you’re pregnant. Congratulations! No doubt, you already have a ton of questions running through your head— What’s so great about the new $1,200 Nuna stroller? How many diapers is too many? Is co-sleeping REALLY that bad (it’s just cuddling on steroids, right…)? These are all exciting topics to dive into as you prepare for the next great addition to your family. But if you’re having a boy, there might be one question on your mind that seems a little more daunting and a little less exciting to have to deal with: What the heck should you do about his foreskin?!
In this post, I’ll give you all the information you need about circumcision—anatomy, history, medical effects, and cultural considerations—in as factual and straightforward a manner as possible, so you can get back to stroller shopping in no time.
—
Anatomy
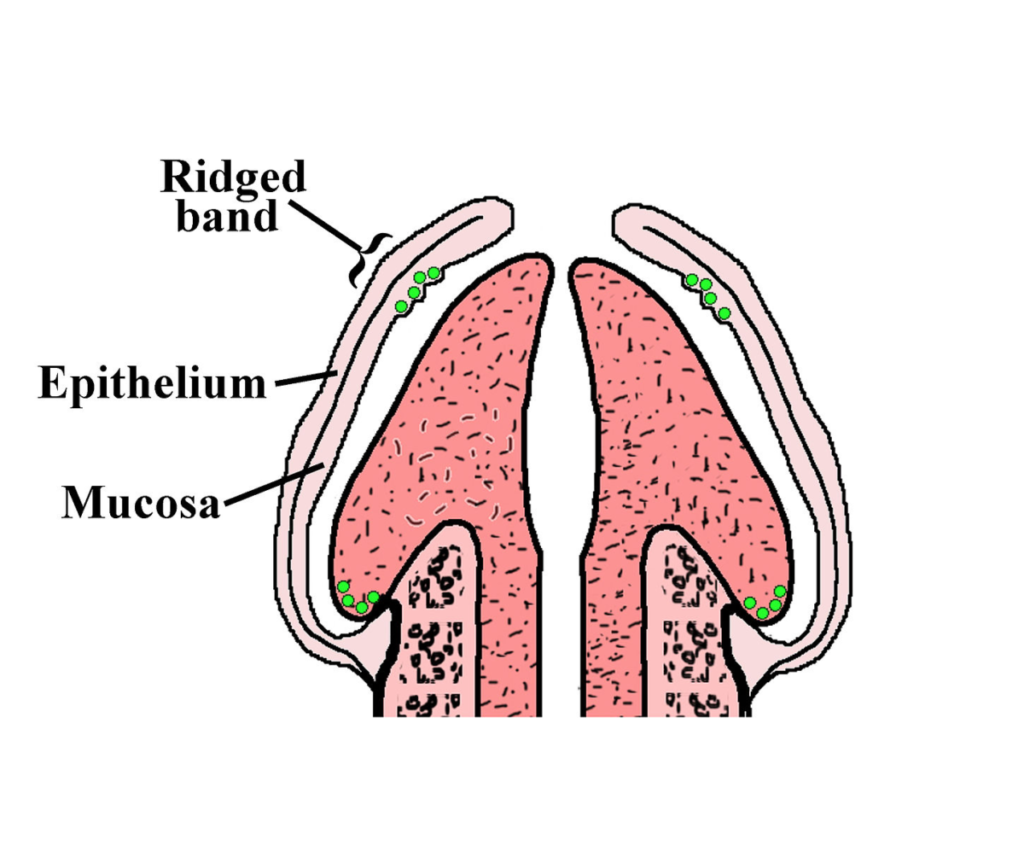
- Male circumcision is a surgical procedure that removes the foreskin (retractable piece of skin) from the head of the penis.
- On average, the skin that’s removed contains more than 3 feet of veins, arteries, and capillaries, as well as about 20,000 nerve endings.
- Foreskin contains the “ridged band”— the heavily innervated mucosal tissue that’s intended to provide natural lubrication during sexual arousal.
- Foreskin protects the head of the penis from friction against clothes. This is important because constant friction can reduce sensitivity, therefore reducing sexual pleasure.
- There’s no clear line of demarcation between the foreskin and the rest of the skin on the shaft penis. This means that there’s no set amount of skin that can or should be removed during a circumcision– the amount that’s removed varies depending on where and by whom the procedure is performed.
Summary: The foreskin is made up of very sensitive tissue that serves a unique purpose in sexual functioning.
—
History
Anthropologists believe that male circumcision could date as far back as 2,300 BCE, to Old Kingdom Ancient Egypt. Since then, it acquired ritualistic value in cultures ranging from Judaism and Islam to tribal Polynesia. In the 1870s, it regained popularity after a few American pediatricians made claims that it cures paralysis and prevents masturbation—which, at the time, was thought to be a great sin, a sign of mental weakness, and the cause of serious illness and death. Though it is not true that the procedure prevents masturbation, more modern science has shown that circumcision can actually have some medical benefits. Let’s take a closer look at those.
—
Medical Benefits
HIV/AIDs:
- It’s well-established that circumcised men are less likely to acquire and transfer HIV under certain circumstances. Such circumstances include lacking access to healthcare, condoms, or soap and water.
- In developed countries such as the United States, circumcision is not an effective preventative tool for HIV/AIDs or other sexually transmitted infections. A far better option would be regular washing and use of condoms.
Penile cancer:
- Penile cancer is extremely rare, effecting fewer than 1 in 100,000 men each year (0.001%).
- Evidence shows that a higher proportion of men with penile cancer are uncircumcised. However, this correlation is believed to be the result of a rare condition called phimosis, which can be prevented through regular washing, and treated with circumcision on an as-needed basis later in life, if necessary.
- In the United States, the average age of onset for penile cancer is about 60 years old. Some other (likely more effective) preventative measures include regular washing of the penis, and abstaining from smoking.
Urinary tract infections:
- In 2012, the American Association of Pediatrics released a policy report stating that in their view, the benefits of circumcision were worth the risks, citing UTI prevention as their primary reason. However, this report received heavy academic criticism for misrepresenting data, and it expired without ever being renewed.
- UTIs are very rare in males, and virtually never occur after the age of two. In contrast, they are very common in women of all ages—at least every other female will get a UTI during her lifetime.
- Approximately 100 circumcisions would be needed in order to prevent a single boy from acquiring one UTI.
- UTIs are very easily treated with a few days of common antibiotics.
Summary: While HIV, penile cancer, and UTIs are statistically significant correlates of circumcision, this does not lead circumcised boys to have better overall health outcomes in the United States.
—
Medical Risks
- Circumcision is usually a quick and safe procedure, though serious complications such as infection arise about 1% of the time.
- Circumcision is a painful procedure, both in the moment and during the healing process. Healing takes about one to two weeks. Local anesthesia should always be used to minimize pain.
- As a boy grows, so will the surface area of his skin. Sometimes the new skin naturally ends up growing back to a length that can retract, leading parents and pediatricians to want to give their boys circumcision “revision” procedures a few years after the initial procedure. While most American insurance companies cover an initial circumcision, most do not cover revisions.
- Circumcision removes a unique structure which contains heavily innervated skin and mucosal tissue, and also protects the glans from excessive friction against clothing. As a result, some research has shown that circumcised men and their partners may experience less sexual pleasure than uncircumcised men and their partners.
- Some circumcised men report that erections, sex, and masturbation are more painful due to a lack of skin, which can cause a feeling of “tightness” and curvature of the penis.
Summary: Circumcision usually does not lead to serious medical complications, but it may lead to decreased sexual pleasure and increased risk of pain from sexual arousal and activity.
—
Cultural Considerations
- Though virtually every American-born male was circumcised soon after birth in the mid 20th century, in recent decades the practice has seen a significant decrease in prevalence. Some states still practice it relatively frequently, but in some states, only 10% of boys are circumcised at birth.
- Since the procedure is not medically necessary, potentially harmful, is conducted on people who cannot consent, and interferes with very intimate body parts and functions, many scholars consider circumcision to violate the principles of bioethics.
- Most other wealthy countries no longer practice male circumcision routinely, and some have made it illegal. In America, too, it’s illegal to perform any genital alteration on female infants, even in ways that are far less invasive than our typical male circumcisions.
- A 2018 study showed that on average, circumcised and uncircumcised men are equally satisfied with their circumcision statuses. However, false beliefs about the practice can impact people’s satisfaction levels.
- Studies show that people’s preferences for circumcised vs uncircumcised sexual partners vary greatly depending on their sexual orientation, past experiences, and where they live.
Summary: Though infant circumcision is still somewhat of a standard in American culture, people’s preferences for it vary greatly across the country, and it receives strong criticism from both American scholars and the general public in most other developed countries.
—
So, do with this information what you will, and go get back to stroller shopping!
—
—
—
References