Our first week in Paris coincided with two championship soccer games. Like many Americans I am unfamiliar with soccer, but our group gathered at a English bar called The Mazet on Wednesday night to watch the Europa League Final: Chelsea vs. Arsenal.
Most of you will be familiar with the ongoing controversy about traumatic brain injury (TBI) in sports. Our national conversation tends to focus on American football, but TBI is also a huge problem in boxing, hockey, and lacrosse (my sport of choice). In the field of medicine, a distinction is made between sports based on the level of risk of injury. The sports listed above are all deemed collision sports, in which “athletes purposely hit or collide with each other or with inanimate objects (including the ground) with great force” (Rice, 2008). Soccer is a contact sport, meaning that “athletes routinely make contact with each other or with inanimate objects but usually with less force than in collision sports” (Rice, 2008).
While watching the game, I noticed that Arsenal’s goalkeeper Petr Cech was wearing a sort of helmet which I later identified as rugby headgear (Rugby is a collision sport). Chelsea’s goalkeeper wore no headgear; neither did either keeper playing in the Champion’s League Final I watched on Saturday night. A fellow patron informed me that Cech had suffered a serious head injury earlier in his career, and had continued to wear the helmet ever since as a preventative measure.
As an American sports fan, I was intrigued. Most players in the sports that I watch are required to wear some form of personal protective equipment (PPE), but very few wear items which are not required. During my years as an athlete, I would often forgo recommended PPE which I found to be unnecessary; most of my lacrosse teammates chose not to wear athletic cups and opted for the elbow pads which were the least restrictive (and therefor the least protective). While the decisions Peter Cech and other athletes make about their PPE mostly come down to personal preference, I became curious about what is being done to tackle (pun intended) the problem of TBI in sports.
Emergency room visits for TBI predominantly involve children, and a significant portion of these injuries are sports related (Sarmiento et al, 2019). This fact seems especially troubling considering the long term effects of TBI and the effects it may have on development are still being investigated. A 2019 study by Russel and Selci administered the Pediatric Quality of Life Inventory (PedsQL) to 134 adolescents who had sustained concussions playing sports. Compared to a control group with non-concussion sports injuries, the experimental group demonstrated severe detriments to their quality of life, especially cognitive functioning and school performance. Patients who had recovered from multiple concussions were significantly more likely to also suffer from depression and headaches (Russel et al, 2019). In this study, after the patients had recovered fully (according to the Post-Concussion Symptom Scale) no longterm neurological symptoms were detected.
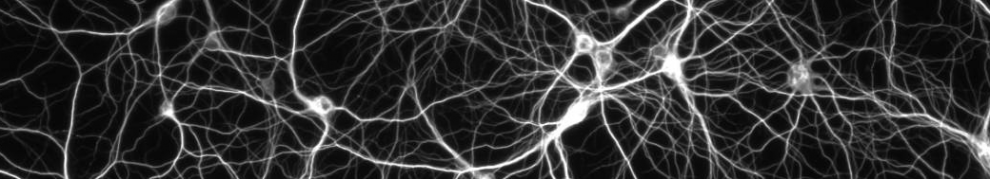
The ongoing media narrative surrounding concussions in sports paints a very different picture from this research. An article published just last month in the New York Times (Branch, 2019) lambasts the National Hockey League for its refusal to acknowledge a link between the sport and neurodegenerative symptoms in its players. Specifically, the article discusses chronic traumatic encephalothopy (CTE), the poorly-understood disease which makes headlines nearly every time a pro-athlete dies. CTE is only diagnosable postmortem and is thought to be linked to repeated TBI (Stern et al, 2019). The disease is characterized by a build up of “tau-aggregates” in neurons, similar to the amyloid-beta plaque build up that occurs in Alzheimer’s disease. In fact, brains in the late stages of CTE also show amyloid-beta plaque deposits (Stern et al, 2019). In a 2019 study analyzing the build up of tau aggregates in the brains of former NFL linebackers, Stern and Adler found significantly more tau aggregate build up in several brain regions thought to be affected by CTE than in non-athletes. However, the increased levels of tau aggregate did not correspond to amyloid-plaque deposit increases or to neurodegenerative symptoms (Stern et al, 2019). To be clear, TBI does have negative effects on one’s health and wellbeing — wear your helmets, kids — its just uncertain how these effects manifest over a lifetime.
Several similar studies seem to debunk the popular narrative that repeated TBI results in severe neurodegenerative symptoms. A 2019 paper by Brett and Wilmoth designed to review the symptoms of CTE and the way that it is diagnosed concluded that the diagnostic criteria are unclear, causing the disease to be over reported (Brett et el, 2019).The high-profile of athletes who suffer from the disease combined with the troubling amount of TBI in children explain why the media, educators, and legislators are all fascinated with combatting a disease that scientists remain uncertain about. Regardless of the effects, TBI is a real risk to athletes the world over. Professional athletes like Peter Cech who are proactive about their safety set a good example for adolescents like me who are making the choice between comfort and protection every time they suit up.
Works Cited
Branch, J (2019) The NFL Has Been Consumed by the Concussion Issue. Why Hasn’t the NHL? New York Times 5/31/2019
Brett BL, Wilmoth K, Cummings P, Solomon GS, McCrea MA, Zuckerman SL (2019) The Neuropathological and Clinical Diagnostic Criteria of Chronic Traumatic Encephalothopathy: A Critical Examination in Relation to Other Neurodegenerative Diseases. Journal of Alzheimer’s Disease 68: 591-608
Rice SG, Council on Sports Medicine and Fitness (2008) Medical Conditions Affecting Sports Participation. Pediatrics 121:841-848.
Russel K, Selci E, Black B, Ellis MJ (2019) Health-related quality of life following adolescent sports-related concussion or fracture: a prospective cohort study. Journal of Neurosurgery Pediatrics 23:455-464.
Sarmiento K, Thomas KE, Daugherty J, Waltzman D, Haarbauer-Krupa JK, Peterson AB, Haileyesus T, Breidling MJ (2019) Emergency Department Visits for Sports – and Recreation – Related Traumatic Brain Injuries Among Children — United States, 2010-2016. Centers for Disease Control and Prevention Morbidity and Mortality Weekly Report 68:237-242.
Stern RA, Adler CH, Chen K, Navitsky M, Luo J, Dodick DW, Alosco ML, Tripodis Y, Goradia DD, Martin B, Mastroeni D, Fritts NG, Jarnagin J, Devous MD, Mintun MA, Pontecorvo MJ, Shenton ME, Reiman Em (2019) Tau Positron-Emission Tomography in Former National Football League Players. New England Journal of Medicine 380:1716-1725



One response to “Traumatic Brain Injury in Sports”