




Current Projects
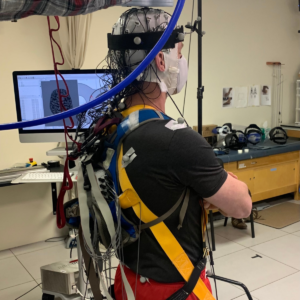
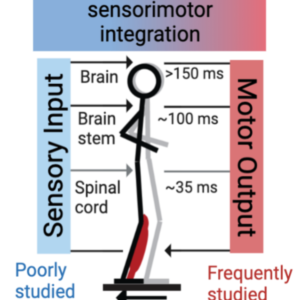
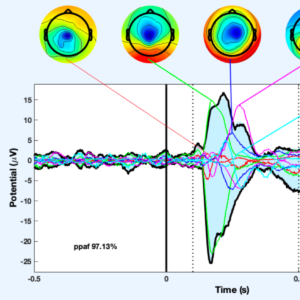
When balance is perturbed, the brain must integrate sensory input across multiple joints and limbs to perceive body position and plan the appropriate muscle response. Findings from our lab demonstrate that stroke survivors have altered cortical responses and muscle activation patterns in response to a perturbation, but it is unknown whether these abnormal responses are related to impairments in whole-body motion perception. In neurotypical adults, whole-body motion perception thresholds vary across individuals, and in older adults, higher (i.e., worse) thresholds are associated with worse balance ability. This research seeks to identify the underlying neural correlates of whole body motion perception and the association to balance ability in neurotypical younger and older adults, and people who have had a stroke. Given increased risk of falls with aging that is further increased post-stroke, developing structural and functional biomarkers of somatosensory perception and balance function is necessary to identify individuals at risk for falls, and to advance development of effective, evidence-based rehabilitation interventions.
We are using measures of ascending nerve fiber transmission/reception and sensorimotor processing in key multisensory regions of the brain to identify markers of proprioceptive deficit and altered visuo-proprioceptive processing post-stroke. The repercussions of (multi)sensory deficit on goal directed action and central processing post-stroke are poorly understood. This project may provide novel measures to advance future sensorimotor research.
Eligibility
1) First-time clinical cortical or subcortical stroke
2) Chronic (>6mo) recovery stage
3) Intact dorsal column-medial lemniscal pathway (SSEP+).
4) Must speak and understand English
5) All participants will need to have normal or corrected to normal visual acuity
This project studies aging-effects on human spatial navigation behavior and their underlying neural correlates in the brain’s spatial navigation network. Specifically, this project aims to assess aging-related deficits in complex, multi-goal, naturalistic navigational behavior and their associations to the connectivity and plasticity of the brain’s navigation network, specifically of the pathway between the hippocampus and the prefrontal cortex, using concurrent TMS-fMRI.
Eligibility:
1) No history of musculoskeletal impairment, neurologic disease, major head trauma, epilepsy, or seizures.
2) No major psychiatric disorder, sleep disorder, or chronic fatigue.
3) No major visual impairments that are uncorrected (if corrected, must be VR-compatible).
4) Right handed
5) Within the specified age ranges for each age group (age: 18-35 years; age: 60+); (6) at least an 8th grade education; fluent in English .
The goal of this study is to uncover new neurobiological influences on how people regain motor and sensory function after a stroke. Specifically, this study will examine the role of global brain health measures, which represent deterioration of systems across the whole brain, in stroke recovery by analyzing both: (a) a large existing database of neuroimaging and behavioral data on stroke patients and (b) new data that will be collected in the first 3 months following stroke, when the majority of stroke recovery is thought to occur. This project is a collaboration with the University of Southern California, Columbia University and The Florey Institute of Neuroscience and Mental Health in Melbourne Australia. The project will create important new knowledge on the relationships of global brain health to post-stroke brain injury, brain repair, and sensorimotor recovery, which can be used to identify novel therapeutic targets to improve stroke recovery.
Eligibility:
Unilateral ischemic stroke within the previous 3 weeks
Arm strength is important for taking care one’s self. Predicting whether arm weakness due to a stroke will or will not improve would allow for more efficient and effective testing of new treatments, and more individualized treatment decisions. This project is supported by the NIH StrokeNet and involves the collaboration of 29 stroke centers across the United States. The VERIFY study will establish the ability of noninvasive transcranial magnetic stimulation and MRI to reliably predict patient outcomes in the important, early period of stroke recovery.
Eligibility:
Unilateral stroke due to ischemia or intracerebral hemorrhage with Motor deficits in the acutely affected upper extremity