
Claudia Morris, MD
Pediatric emergency medicine physician, research director for the Center of Clinical and Translational Research, professor of Pediatrics and Emergency Medicine at the Emory University School of Medicine, and chief investigator for the Pediatric Emergency Care Applied Research Network. These are only a few of the many hats that Claudia Morris, MD, wears as she works to improve the lives of her patients, students, and those impacted by her clinical research.
Morris has been involved with clinical and translational research for over 25 years. In her words, it has been “quite a journey.” That said, she didn’t intend to be a clinician-scientist at the beginning of her medical education pathway. She started with the intention of being a clinician in one of the high-energy subspecialties such as emergency medicine, critical care, or pediatric hematology/oncology. At the time, Morris didn’t think research would be a part of her long-term medical career.
A transformative research experience
This perception changed when she took a job during her two-year gap between college and medical school. Her first job out of undergrad was at a nitric oxide lab in New York, and it was there that she was first exposed to the impacts of arginine (an amino acid that the body uses to regulate blood pressure and T cell function/immunity) and nitric oxide on biological mechanisms — key information that would guide her sickle cell disease (SCD) research ten years later.
“I didn’t realize at the time that I had the fire in my belly to do research,” said Morris.
Even though the lab was working with animal models, she was always asking, “How could this apply to humans?” She considers her time at the nitric oxide lab to be an “unexpected twist of fate” because the experience ultimately transformed her career.
Though Morris is a clinician by training, she is more accurately a clinician scientist with a focus on arginine and nitric oxide research. Her early lab experiences sparked her interest in translational research (i.e. applying research findings to create products or change practices to benefit patients and the general public) and taught her how to “speak the language” of the medical scientists. Even so, she consistently pushed for answers about how the research can impact patients.
A revelation from a simple observation
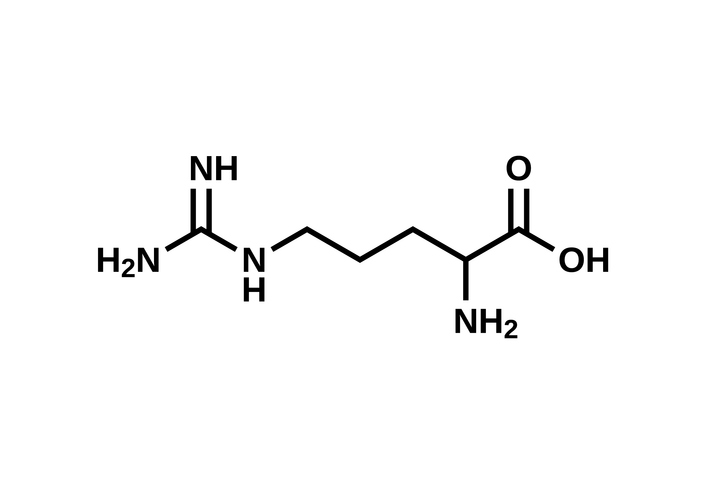
Amino acid arginine structural formula, C6H14N4O2
Because of her work in the nitric oxide lab, Morris was able to make connections about arginine and sickle cell disease that she may not have been able to otherwise, as such knowledge is not common for emergency room physicians. In fact, she considers one incredible discovery to initially be “a simple observation.”
She was at a conference presenting her fellowship research project when she saw a poster about research linking complications of SCD and nitric oxide bioavailability. Morris considered her critical knowledge about the connections between arginine and nitric oxide she obtained at the New York lab. This conference inspired her to pursue her own literary research into arginine dysregulation, and she learned that arginine levels were typically found to be low in SCD patients.
At the time, the mechanisms for arginine deficiency were not clear, but Morris, who was completing her training at the UCSF Benioff Children’s Hospitals in Oakland, Calif., received a small pilot from UCSF to conduct her research. Blood samples from hospitalized pediatric SCD patients confirmed that the acute pain they experienced was associated with an arginine deficiency.
After receiving funding from the NIH via the K23 Career Development Award, Morris sent her preliminary data to multiple clinical trials of arginine as a nutritional supplement. The trials found that arginine supplementation increased the quantity of nitric oxide metabolized in the blood. Even more astonishing, the study showed “this nutritional supplement decreased total intravenous (IV) opioid use by 55%, and significantly reduced pain scores at discharge. It also showed trends of decreased length of hospital stay” (Emory Medical School). Basically, the trials finally provided a sustainable solution for the debilitating pain of pediatric SCD patients: treating them with an amino acid supplement instead of opioids.
Above: Photos of Morris with her mentees winning awards, presenting research, and participating in teambuilding activities.
Further trials and possible supplement therapy
The implications of the studies are astounding in that further research could yield a far healthier alternative treatment for children experiencing pain as a result of SCD. It’s the difference between treating the patients with an amino acid supplement and treating them with opioids. The National Institute of Health awarded Emory University a $8.7M grant to perform a phase three trial entitled Sickle Cell Disease Treatment with Arginine Therapy (STArT trial) to definitively confirm the correlation between arginine supplementation and decreased pain. Funding for early-stage biomedical research is a rarity. For Dr. Morris, to receive such a grant from the NIH means that they recognized the dire importance and potential lasting impact of her work.
Long-term, Dr. Morris’s goal is to “develop a drug that will improve pain [in SCD patients] and [can] be initiated in the emergency department.” Further, if her current STArT trial is successful, she plans to work with the FDA to implement arginine supplement therapy nationwide so that the therapy can be used to help as many people as possible. Additionally, her work with arginine has further applications for children hospitalized with COVID-19, which has a few overlapping effects with SCD. She hopes to receive funding so that she may further research arginine intervention therapy and how it could be used to treat patients affiliated with other diseases that could be the result of arginine dysregulation.
A strong network of support

Morris and her husband
When asked how she balances her many professional duties with her personal life, she credits her husband and three children for keeping her grounded and supporting her the whole way, even moving from California to Atlanta when Morris was recruited to Emory.
“Having an understanding support system is key!” Morris stated.
Further, the role of a clinician-physician is not an easy path, but having a talented team to delegate to allows for increased productivity and efficiency and decreased stress. “I have an amazing team and people who have been helping me move forward so that we’re even more productive.” Regarding her work, she said, “You can feel like you’re pushing the boulder uphill, and if you don’t have champions around you to remind you of why you’re doing it, then you never get to the endpoint. But when you’re making discoveries and changing practice, nothing compares to that.”
— Jenna Woods




