by Drew Lawless
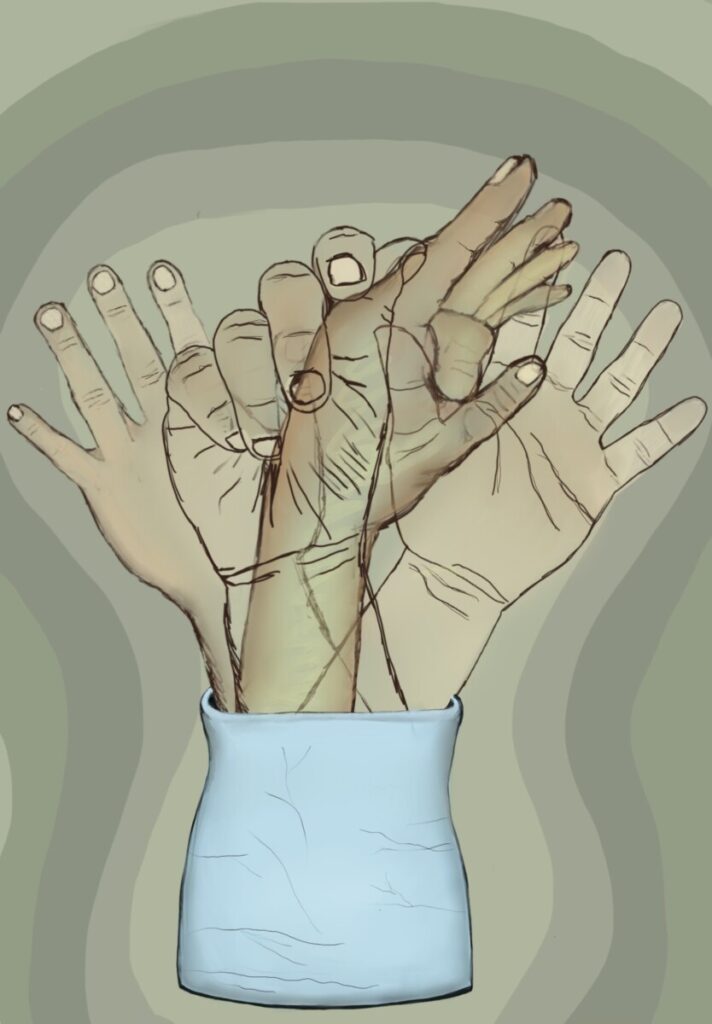
art by Charlotte Kaufmann

Without warning, our minds have the terrifying power to separate us from being in focus to swimming in a sea of disorientation. This feeling, known to most as “dissociation,” is a bodily response that causes one to feel disconnected from their thoughts, emotions, and surroundings, which can be a startling and abstract experience. Sometimes, this cognitive response can go beyond its general function; this is the area of dissociation that can be officially recognized as a disorder. This article aims to explain the neuroscientific perspective of why dissociation occurs, what causes it to go haywire in the form of a disorder, and how it varies from person to person.
The origins of the documentation and study of dissociation can be traced as far back as the late 18th century. Only after the Vietnam War in the late 1970s was dissociation truly recognized as a legitimate psychological state of being. Over time, it also began to be identified as a common symptom of other mental disorders [1]. This was primarily due to dissociation being tied to post-traumatic stress disorder, or PTSD for short. This disorder is now known to be heavily influenced by dissociation, mainly due to how it was seen to confuse the traumatic event (such as gunfire or an explosion) with non-traumatic, everyday stimuli (such as a car backfiring) [2]. The sounds and sights of wartime carried over into certain veterans’ post-war lives, leaving them to suffer through an unknown “out-of-focus” sensation when triggered by their environment [2]. Following this period, various tests and DSM (Diagnostic and Statistical Manual for Mental Disorders) classifications were developed for the “subcategories” of dissociation and disorders that have it as a major symptom. It has now become a major source of psychological research and inquiry [1].
Unfortunately, dissociation is still a relatively unexplored field of neuroscience. Consequently, psychologists and therapists lack the knowledge to fully accommodate the needs of their patients. There is not much general knowledge on dissociation, as well as no true definition of the condition. Such a large variety of related symptoms and perspectives exist that it is difficult to pinpoint what it exactly means to dissociate or have a dissociation disorder [1]. Generally, however, dissociation can be grouped into two separate sub-experiences: depersonalization and derealization. Depersonalization describes “out-of-body” moments, while derealization is associated with “out-of-focus” moments. These sub-experiences range in terms of how extreme they are, how often it is noticed in varying individuals, along with all the other symptoms experienced during dissociation.
From a physiological perspective, dissociation is the human body trying to protect us from negative external or internal stimuli. This can be in the form of a stressful situation or general anxiety. From a neuroscience perspective, research points to the brain’s fear response and emotion-processing centers as the primary cause [3]. The lack of signals being sent and relayed to other brain regions prevents the individual from being able to comprehend what is actually happening. Electrical signals from active brain cells, or neurons, are slowed down. This means that fewer activating messages or commands are being sent to these regions and that they take much longer to reach their designated target. Thus, they have no lasting effect on this region of the brain known as the “Cortico-Limbic System,” the portion of the brain that associates our thoughts or awareness with our emotions [3]. The overarching result of this is a lowered sensory awareness of one’s self and their surroundings [3].

What happens, however, when this natural response occurs without a reasonable or legitimate stimulus? This is where general dissociation turns into a dissociative disorder. Various dissociative disorders exist, but three very prevalent disorders worth focusing on are dissociative amnesia, depersonalization-derealization disorder, and dissociative identity disorder. While plenty of other mental disorders are involved with dissociation, these three, in particular, showcase very explicit and/or extreme dissociative symptoms.
Dissociative amnesia is categorized as an unusual inability to recall information or memories related to a traumatic or stressful event in one’s past. It is usually developed in response to trauma at a young age, mainly due to how critical those years are for our brain’s development [4]. However, there are, of course, instances of adults experiencing severe trauma and developing the disorder as well. This is because the person’s mind works extra hard to shut out the traumatizing stimuli, to the point that it is quite debilitating and prevents easy memory retrieval related to that time or event [4].
Depersonalization-derealization disorder is just like it sounds: it features extreme, maladaptive cases of both depersonalization and derealization symptoms. The person diagnosed might feel lifeless or aimless, as if they were watching a movie of their life instead of actually experiencing it. Obviously, they are still conscious, active humans, but they internally function much differently when going through an episode of the disorder [5]. The symptoms can be brought on by the biological response to stress or for no apparent reason; however, it is kicked into overdrive and makes the observer hyper-aware of their “trance-like” state [5].
Dissociative identity disorder, easily one of the most interesting and debated mental disorders, is what was once referred to as “multiple personality disorder.” It can be defined as the creation of alternate “senses of self” that appear to most outside observers as distinct personality changes. This occurs in response to intense childhood trauma, abuse, or neglect, mainly to protect the original personality from the stressful stimulus or pain being suffered. The dissociation aspect specifically involves the mind, causing the original personality to forfeit control of the body and awareness of their surroundings to an alternate personality [6]. This is not a voluntary action by the primary self; to them, it is as if time has skipped forward, and they have no memory of what happened between their last thought and now. Of course, this changes for everyone who has the disorder, but some very extreme cases, such as someone having 27 personalities, have made the illness a major cultural spectacle. Psychologists and neuroscientists have studied the illness for decades. Despite the major belief that it was not a real disorder, based on more recent scientific evidence, it has been proven to have a biological basis as a legitimate chronic disorder [6].
In regards to these and other disorders related to dissociation, treatment is a feasible yet abstract process for those suffering through its wide range of symptoms. No specific medication is available to target areas of the brain responsible for dissociation, and there is not one definitive therapy option or style in use. However, a mixture of various therapeutic strategies and particular medicine available can improve one’s well-being [7]. Common examples of this include talking through the traumatic stimulus that causes the symptoms with a licensed therapist or psychiatrist, learning how to bring oneself back into focus when dissociating with a strategy called “grounding,” and regulating the stress itself with medicine [7].
Since most disorders related to dissociation involve issues with the body’s stress response system, antidepressants, anti-psychotics, and anti-anxiety medications can help lower the afflicted mind’s natural tendency to pull one’s consciousness away from their surroundings. The intended result of this is to lessen the severity of the dissociative symptoms and their frequency. Neurotransmitters, chemicals responsible for changing the electrical activity (or inactivity) of certain brain regions, are the main focus of these medications [8]. These include serotonin, which controls mood; dopamine, which controls feelings of reward and happiness; GABA, which inhibits anxiety or stress; and glutamate, which controls learning and memory [8].
Current research on dissociation is done with attempts to find the more accurate source of dissociative problems in the brain. A recent study from Stanford found interesting evidence pointing to new areas of the brain and even our cells that might be the root cause for these dissociative feelings. More specifically, these are the posteromedial cortex, which controls subjective thought, and ion channels on the cell membrane, which control the sending of signals via neurons. By stimulating and/or accessing these regions of the body in humans diagnosed with epilepsy (those with recurrent seizures), they experienced mild dissociation but no seizure whatsoever [9]. Although this might not be a complete solution to the dissociation symptoms, this research can provide great assistance in understanding mechanisms of neural signaling that can also cause dissociation when underactive, compared to being overactive as seen in Epilepsy. We now also have a better idea of where to look for the cause of dissociation [9].
Due to the complex nature of dissociation, there is not one correct answer. Despite these unfortunate circumstances, there are various means to seek help for symptoms. The amount of research available on dissociation is inadequate to properly understand and treat its many facets. With time, resources, and continued support for the neuroscience community, there is great hope for what can be discovered and done for those dealing with any form of dissociative and related disorders. What can be done now is informing oneself on what people go through with these unfortunate dissociative mental disorders. Although the average person can’t change dissociation in a single night, it helps tremendously to be aware of dissociation in general and how prevalent it actually is in human life.