Changing Relationship
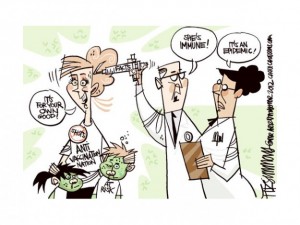
In the past, the physician patient relationship was one of complete trust. Physicians thought they knew everything about medicine, and patients had few other ways of gaining information so they did as they were told. The relationship was deeply rooted in paternalism. However, the influx of medical information readily available in our society as well as a new emphasis on personal care is driving patient empowerment. In addition, the limited time physicians have to spend with their patients have led to less personal relationships and a dramatic decrease in listening to the patient’s concerns and problems. In our time, physicians have little knowledge of their patient’s desires, mentality, and values, which can affect the way they administer treatment. One study even showered that resident doctors spend 12% of their time interacting with patients compared to 40% of their time interacting with the computer. It is difficult to form relationships with patients in this small window of time.
Role of Consent in New Relationship
Robert Veatch argues that consent it a transition concept, an innovation that is only useful as a transition to a more thoroughly revisionary conceptual framework. Veatch argues that with the little information physicians truly know about their patients, their personalities, and their values, there is no way that they can even guess what is in the overall best interest of the patient. Veatch believes that in order for a physician to guess what is the best course for the patient, three assumptions must be true regarding a theory of the good.
- The physician must determine what will best serve the patient’s medical interests.
- The physician must determine how to trade off health interest with other interests.
- The physician must determine how the patient should relate the pursuit of his or her best interest to other moral goals and responsibilities that may conflict.
In our day and age, Veatch believes it improbable to expect a typical medical professional to be able to fulfill even one of these, let alone all three. In addition to arguing that since a physician has little relationship with the patient, they often cannot accurately determine what is in their best interest, Veatch also argues that physicians are only experts in one component of well-being (medical) and therefore are unable to determine what constitutes the good for another being.
Where Do We Go From Here?
Veatch argues that there are two alternatives to informed consent. The first option being to emphasize the concept of choice rather than consent. Since physicians have no way of knowing what is in the patient’s best interest, they should present the patient with a list of plausible treatment options with the potential benefits and risks of each, allowing the patient full autonomy and choice in their course of action. This seems extremely implausible. A more realistic, but still a stretch, of an option is pairing physicians and patients based on their “deep interests” including religious and political affiliations, philosophical and social inclinations, and other worldviews. This would put both provider and patient on the same page of what values are necessary and essential part of health care decision making and allow physicians to provide the course of action that best falls in line with patient’s views and values.
To me, these two alternatives seem a little farfetched. I think where we need to start is by changing the paternalistic physician-patient relationship to more of a partnership. Physicians need to embrace listening, and think of themselves as more of a health coach then the end all and be all of medical knowledge.