This past weekend, our group went to Provence, a province in southeast France, and visited the city of Arles where Vincent van Gogh lived for two years painting some of his most famous works such as Yellow House, Starry Night Over the Rhone, and Bedroom in Arles.
Before going there, we saw in class the movie, Lust for Life, a 1950’s biographical movie about Vincent van Gogh’s life highlighting his interactions with other painters, his family, and his surroundings (Lust for Life – Trailer, n.d.). The movie touches on Van Gogh’s lifelong mental strife showing that while we revere him as an artistic genius now, very few people understood him including himself.
It seemed the depression that Van Gogh experienced subsided according to his letters to his family and friends, but in the movie, they show the manic way he painted constantly covered in paint and obsessed with catching the light to paint landscapes and field laborers. When the fall and winter came around, he could not go outside expressing how he felt trapped. His condition worsened where outside painting did not work anymore leading up to him to cut off his ear with a variety of possible reasons that no one could confirm. He eventually was admitted to a hospital where his hallucinations continued with blocks of time missing from his memory and his alcohol abuse addressed. He still continued to paint famous pieces such as The Courtyard of the Hospital at Arles 1889 that are preserved to this day.
We looked at his doctor’s notes categorizing his condition as epilepsy because of his ongoing non-lucid episodes, so we started looking into different mental conditions that related back to the ones we know today as major depression disorder, bipolar disorder, schizophrenia, and more. This eventually led us to see what type of treatments would be available for the people with dementia praecox: a term coined by Emil Kraepelin to describe lesions in the cerebral cortex that mild dementia (Adityanjee et al., 1999). I couldn’t find much in terms of treatment, but it got me thinking about what we have today to help alleviate the effects of mental illnesses such as bipolar disorder, schizophrenia, and depression. As well as my interest being piqued through exploring Van Gogh’s life, there is a high probability I will see these novel practices implemented in the future.
The School of Nursing at Emory does a good job of teaching us the evidence-based practices that we follow for patient safety and comfort, but the patients have the autonomy in most cases to deny treatment, do something different than recommended to treat their ailments , or ask about new upcoming treatments. Because of this, it is important to know recent research about various types of treatment practices to be better support the patients.
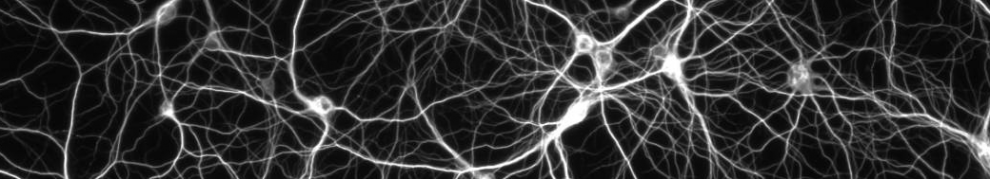
One that was really interesting to find out was the possible implementation of brain-derived neurotrophic factor (BDNF) to help treat neurodegenerative diseases as well as mental health disorders. It is a growth factor that is used in neurogenesis or the formation of new neurons which is not common for adults; in most of the brain, there are no new neurons created from the ones at birth, but there are some brain areas that still have new neurons created which is where growth factors like BDNF are used those new neurons (Bathina and Das, 2015). This is also used for synaptic plasticity in which there is a consistently strong or diminished communication between the neurons depending on how strength and importance of the signal is between the two neurons (“What Is Synaptic Plasticity?”). There is also evidence that a depleted amount of the class of factors BNDF belongs to can possibly be an indicator for neurological disorders such as Parkinson’s disorder and Alzheimer’s (Bathina and Das, 2015). While BNDF has the ability for synaptic plasticity, a study done with mice found that inhibition of one of the receptors BNDF can bind to shows a decrease in long term depressive behaviors without affecting its synaptic plasticity function in other brain areas (Woo et al., 2005). Researchers also theorize that people with reduced BDNF levels might have a decreased synaptic plasticity in the hippocampus which prevents the body from going back to homeostasis taking them out of their stress related depressive states (Phillips, 2017). The second type of receptors that BDNF does the opposite effect by producing synaptic plasticity; this receptors’ activation and an BDNF increase is seen in the presence of certain antidepressive pharmacologic therapies (Phillips, 2017).This is now being used as an indicator for future drug therapies as a measure of effectiveness.
Going away from the pharmacological side, I started to think about Van Gogh and how his art was a source of peace and strife for him. At some point, painting couldn’t help in him in the way it did before. This is not to discredit the effects that art and other alternative therapies have on supporting those with symptoms similar to his; a study had 58 patients diagnosed with schizophrenia do art therapy twice a week for twelve weeks (Montag et al., 2014). They found that those who had committed to the program had less negative symptoms which include a loss of interest and a lower affect as well as less positive symptoms of schizophrenia such as auditory hallucinations compared to the control group who did not receive the art therapy (Montag et al., 2014) (“Symptoms,” 2017). This support the idea that Van Gogh’s art was a therapeutic event for him up until everything became too much. It’s fascinating to how we reverie Van Gogh’s coping mechanism after his death with his few family and friends supporting his ability to paint. It makes you think about those that we have forgotten about who are tucked away in our society creating the next artistic masterpiece of our time.
References
Adityanjee, Aderibigbe, Y. A., Theodoridis, D., & Vieweg, W. V. R. (1999). Dementia praecox to schizophrenia: The first 100 years. Psychiatry and Clinical Neurosciences, 53(4), 437–448. https://doi.org/10.1046/j.1440-1819.1999.00584.x
Bathina, S., & Das, U. N. (2015). Brain-derived neurotrophic factor and its clinical implications. Archives of Medical Science : AMS, 11(6), 1164–1178. https://doi.org/10.5114/aoms.2015.56342
Lust for Life – Trailer. (n.d.). Lust for Life – Trailer. Retrieved from https://www.youtube.com/watch?v=WUHL0h_kQ6s
Montag, C., Haase, L., Seidel, D., Bayerl, M., Gallinat, J., Herrmann, U., & Dannecker, K. (2014). A Pilot RCT of Psychodynamic Group Art Therapy for Patients in Acute Psychotic Episodes: Feasibility, Impact on Symptoms and Mentalising Capacity. PLoS ONE, 9(11). https://doi.org/10.1371/journal.pone.0112348
Phillips, C. (2017). Brain-Derived Neurotrophic Factor, Depression, and Physical Activity: Making the Neuroplastic Connection. Neural Plasticity, 2017.https://doi.org/10.1155/2017/7260130
Symptoms. (2017, October 23). Retrieved June 10, 2019, from nhs.uk website: https://www.nhs.uk/conditions/schizophrenia/symptoms/
What is synaptic plasticity? (2016, November 22). Retrieved June 9, 2019, from https://qbi.uq.edu.au/brain-basics/brain/brain-physiology/what-synaptic-plasticity
Woo, N. H., Teng, H. K., Siao, C.-J., Chiaruttini, C., Pang, P. T., Milner, T. A., … Lu, B. (2005). Activation of p75NTR by proBDNF facilitates hippocampal long-term depression. Nature Neuroscience, 8(8), 1069–1077. https://doi.org/10.1038/nn1510
Picture #1: [Screenshot of the walking tour of Van Gogh’s art in Arles]. Retrieved from https://www.google.com/maps/d/u/0/viewer?mid=1014-AkOjbBzXEQQLcxz8NGxa10Oo1bGN
Picture #2 and #3: Taken by me
Picture #4: Painted and picture taken by me