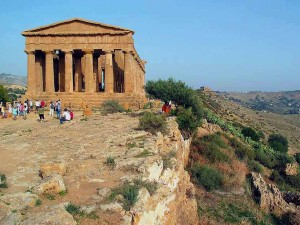
This summer I studied abroad in Italy, and in six weeks, I traveled to over 40 cities. We didn’t have a traditional classroom setting for the streets of Rome, the museums of Pisa, the temple of Agrigento (in Sicily), and even the seats of our bus, winding through the Tuscan hills, served as our classroom.
One of the two courses we took was called Medicine and Compassion, and our professors were from the CDC and Emory Medical School. I thought our professor must be “science people” and we would just talk about medicine because what could you teach about compassion other than to have it?
Looking back, I laugh at my former self for my naivety. In this class, we read a few books, several short stories, and many articles that highlight compassion, empathy, communication, and ethical dilemmas. We were constantly asked, “what is compassion?” I began in Rome thinking compassion was feeling bad and being nice to a person who was dealing with a difficult thing and trying to put myself in their shoes. Wait isn’t that empathy thought? I was very confused and continued to be. My definition changed weekly with new insight gained and old preconceived notions lost. By the end of the program, my definition of compassion included the ability to connect at a personal level despite not having been in their situation and being able to communicate with them so that they could understand me and I could understand them.
You may think, “What does compassion have to do with informed consent?” Don’t worry; I’m getting there! Informed consent relies on physicians educating their patients and explaining what is wrong with them, the risk of a procedure, or their prognosis. In the article “Should informed consent be based on rational beliefs?” the author states “physicians duties as educators are more extensive … physicians must be prepared to do more than provided patients with information relevant to making evaluative choices. They must attend to how that information is received, understood, and used”.
I used to, and I am sure many physician still today, believe that you just need to tell the patients the facts. What could be so hard to understand? It is very easy for people to forget that not everyone knows or comprehends their field, and this is particularly true in medicine. Furthermore, physicians and other professionals alike are at the top tier of the education spectrum and there are many patients who did not go to college or even graduate high school. Those patients ability to understand medical terminology and the implications of treatments is much more limited. Thus, it requires the physician to have compassion and educate the patients to obtain true and complete informed consent.
Below is a link to an article in the New York Times called “Can Doctors Be Taught How to Talk to Patients?” I think this article, like my study abroad program, demonstrates the medical communities recognition and refocusing on the doctor-patient relationship and what exactly that should entail. According to the NY Times article “after all, [doctors] admission to medical school was not based on a validated assessment of their ability to relate to other human beings.”
References:
Savulescu, Julian. and Momeyer, Richard. “Should informed consent be based on rational beliefs?” Arguing About Bioethics. Ed. Stephen Holland. London: Routledge, 2012. 332. Print.