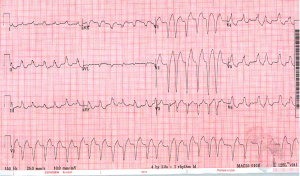
A 60 yo male came into Midtown a few days ago for generalized weakness. He was hemodynamically stable and the EKG above was obtained. With an irregularly irregular wide complex tachycardia like this our differential is fairly short…
1) A-fib or MAT with aberrant conduction (aka a bundle branch block)
2) A-fib or MAT with conduction via accessory pathway (aka WPW)
3) A-tach or A-flutter with variable block and aberrant conduction
4) A-tach or A-fluter with variable block and accessory pathway
So how do we tell the difference? And does it matter, or should we just treat them all the same to avoid making mistakes? In the unstable patient electricity is always the answer, but in stable patients you can go in a few different directions.
If you felt confident that this was Afib/Aflutter with aberrancy you might consider rate control with a nodal blocking agent, but you risk dropping their BP with diltiazem or metoprolol, and if this is in fact Afib with WPW nodal blocking agents could cause increased conduction through the accessory pathway initiating Vfib.
if you think this is WPW procainamide is your first line choice. In theory this will only slow conduction through the accessory pathway, but in reality there is also a high likelihood you will convert the patient back to a sinus rhythm. This could cause an embolic event just like electrical cardioversion. Also this is a high stakes scenario and it is hard for me to reach for a drug I have only given a handful of times.
My thought is unless you have a good reason not to shock, synchronized cardioversion is the way to go for all wide complex irregular tachycardias. In a high stakes situation, it’s good to stick to what you are most comfortable with. For me, that’s 0.15 mg/kg of etomidate, and 100-150J of synchronized cardioversion. Of course there are always exceptions and a good history from the patient might change the direction I go in, but when it doubt… shock! Curious to hear everyone’s thoughts…

4 comments
Skip to comment form
I agree, completely. Synchronized electrical cardioversion at 100-200J with biphasic machine is safe for all unstable tachycardias, regardless of wide or narrow (barring an obvious sinus tachycardia).
It’s my opinion that giving adenosine to any regular complex tachycardias whether narrow (SVT) or wide (VT, SVT with aberrancy, AT with aberrancy) is safe. Obviously, Adenosine is not effective in VT but sometime it is hard to differentiate SVT with aberrancy and VT. That being said, regular complex SVT’s with aberrancy involve the AV node is some portion of conduction making adenosine helpful in breaking the circuit. Check out this link on the Brugada criteria: http://lifeinthefastlane.com/ecg-library/basics/vt_vs_svt/
The real danger in nodal blocking agents is with irregular wide complex tachycardias such as afib with aberrancy like the rhythm you present. Although electricity is safe, I think residents should become familiar with procainamide and ibutilide. The dose of procainamide is 15 mg/kg IV x 1 then 1-4 mg per min maintenance. A great article on AFib in WPW and how to become familiar with procainamide and ibutilide by Fenger, Brady, Plautz American Journal of Emergency Medicine (2007) 25, 576–583
That’s just my 2 cents! I’m sure this is going to elicit some conflicting opinions.
In discussions with cardiologists at the same clinical site, better to shock. Faced with a similar situation years ago, I tried rate and rhythm control pharmacologically for hours on a patient with borderline blood pressure. I asked our EP attending what he would do, and he said “shock.” In fact, when I suggested the patient go to the EP lab, he came down to the ED, and administered the shock himself.
Patients that have short duration AF have <1% chance of having an embolic thrombus. Patients with longer duration AF have a significantly higher risk of thrombus, but still maintain an overall low risk for thromboembolic event. The patient described here, while not hypotensive, sounds hypo perfused. I think the risk of leaving this borderline unstable rhythm untreated is much safer than the single digit risks of cardioversion.
If you wanted to be extra-safe, get or do an echo prior to shock.
We, as ED docs, forget that the highest risk for the patient for thrombus formation is actually after return to sinus rhythm in these patients, usually due to myocardial stunning. The recommendations are for 4 weeks of anticoagulation after conversion to sinus.
Adenosine is a safe alternative in monomorphic Vtach and will convert some 20 odd percent of cases of Vtach. Sometimes its al alternative while your getting out the pads. Is is not that case(irregular and polymorphic) but thought its an interesting concept.
If the etiology of the rhythm cannot be determined, the rate is regular, and the QRS is monomorphic, recent evidence suggest that IV adenosine is relatively safe for both treatment and diagnosis (Class IIb, LOE B).