Radiation Risk:
Average US background radiation in one year: 3 mSv
CxR: 0.02 mSv Pelvis XR: 0.7 mSv
CT Head: 2mSv CT Chest: 8mSv CT A/P: 10mSv
Cardiac PET: 14mSv
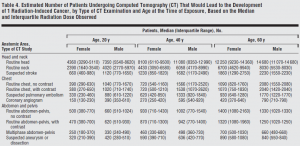
So what is the risk for cancer? It varies by study type, age, and sex. So for example, if a 20 yo F gets a CT abdomen and pelvis with contrast, that CT scan increases the patients risk of cancer by 1 in 470 or 0.2%.
Bindman et al. ARCH INTERN MED/VOL 169 (NO. 22), DEC 14/28, 2009
http://hps.org/documents/meddiagimaging.pdf

3 comments
I am delighted to see this blog on medical radiation doses. I want to make a few comments:
1- the 3 mSv annual dose is from exposure to natural radiation primarily emitted from radon and cosmic rays.
2- If you add non natural sources of radiation then the annual dose in the US on average is 6.2 mSv based on the latest NCRP report. published a few years ago.
3- One should not attempt to estimate a cancer risk increase in an individual patient from a single study. The conversion formulas used to go from a CT scan dose to a cancer risk increase use cancer risk estimates from exposure to doses higher than the doses delivered for medical diagnosis.
The cancer risk increase is also based on a population excess cancer risk over a life time.
4- that said, optimizing doses delivered during imaging is very important. Similarly, imaging wisely and enhancing our clinical judgement as best as possible can mitigate unnecessary exposure to radiation and is in harmony with the ALARA principle (As Low As Reasonably Achievable).
Thank you for the opportunity to contribute to this blog.
Ziad Kazzi
Dr. Kazzi makes all excellent points.
I’ll just add that it’s rational to be very skeptical of studies published that make claims about the number of expected cancers from medical diagnostic imaging. There are tremendous limitations to the modeling and math used to make those predictions. And the predictions can at best be used on a population level, the math gets even more dicey if you try to extrapolate to the risk for an individual from a single study.
In my practice, I tend not discuss risks from radiation in terms of numbers with patients because I don’t feel there is a solid number to quote them. If a patient is worried about radiation I try to elicit their concerns and focus the discussion around the reason I think they need the study.
While there is no solid number that represents the cancer risk to a person from say, a CT PE, I’m confident that it’s got to be way less than 1%. So if I feel my patient has a chance of PE that is at least 1% then this aspect of the risk:benefit ratio is favorable to do the study. Now, I don’t advocate scanning patients who have a 1% chance of PE, but the example illustrates one way to think about this radiation-risk issue.
great website reference:
http://www.xrayrisk.com/
use it on your shift to help conceptualize the increase lifetime cancer risk that you expose your patient to.