EMory Files
Case #6: Beta Blocker Overdose
Hx: 70 yo presented with AMS s/p seizure. BS 35 in field
PE: VS: HR39, RR 10, 80/40, O2 98% RA. After 2 amps of D50 àBS 130. Mental status: wakes up to follow commands but falls asleep quickly.
Beta Blocker Toxicity
***Case Discussion with Dr. Kazzi***
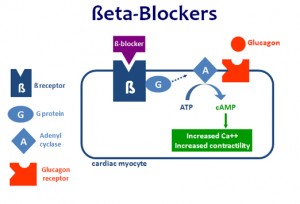
1) What is the mechanism of BB toxicity? Receptors Beta1: Cardiac Beta 2: smooth muscle in lungs and around blood vessels. Beta blockers prevent the production of cAMP. cAMP is critical to the release of Ca++ from the sarcoplasmic reticulum and contraction of muscle. (http://i.imgur.com/Nk9cRh5.jpg)
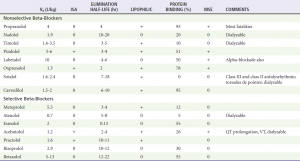
2) Are some BB worse than others? Although selectivity for cardiac receptors is lost in overdose, not all BB are the same (see chart below). Propranolol is the most fatal because of it’s liphophilicity which allows it to penetrate the CNS and it’s extensively protein bound which prevents it from being dialyzable.
Cole JB, Roberts DJ. Cardiovascular Drugs. Rosen’s Emergency Medicine: Concepts and Clinical Practice, 7th ed., by J.A. Marx et al., 2014. Editors: Hockberger RS, Marx JA, Walls RM, Rosen P. Saunders Publishing Philadelphia, PA. 2014
3) Are there toxicites that present similarly? CCB’s. Verapamil and Diltiazem are cardioselective whereas dihydroperidines like Amlodipine target smooth muscle. Regardless, they target L-type Ca+ channels which, subsequently, triggers release from the sarcoplasmic reticulum. This Ca+ release is critical to phase 2 of depolarization in cardiac conduction cells and contraction in smooth muscle tissue. Hyperglycemia in CCB overdose results from blockade L-type Ca+ channels in the β islet cells. Insulin euglycemia therapy (1U/KG IV regular insulin with 0.5 g/kg dextrose) delivers carbohydrates to depressed cardiac cells improving their function.
4) Management: First line treatment
- IV, O2, Moniter, 20cc/kg IVF Bolus
- Glucagon: 3-10mg IV x1 followed by 3-10 mg per hour (watch out for vomiting)
- Calcium: 3-6 g Ca Gluconate over 10 minuts
- Insulin Euglycemia Therapy (1U/KG IV regular insulin with 0.5 g/kg dextrose)
- Pressors (Isopreteronol, norepinephrine, epinephrine)
- Atropine: effective prior to vagal stimulating procedures such as intubation, NG, or gastric lavage.
5) Management: Standard Approaches (Limited Evidence)
- Charcoal: 50-100g x 1 PO within 1 hour of ingestion and NL Mental Status
- Gastric Lavage: Large (1g) overdose within an hour of ingestion
- WBI: 2L/hr GoLytely in sustained release ingestion
6) Management: Advanced options
- Transvenous pacing limited evidence
- Dialysis only in hydrophilic non-protein bound beta blockers
- Intralipid experimental, consult Toxicologist
- Intra-arterial balloon pumps limited evidence
Case Resolution:
Patient responded to glucagon 3mg IV. She was started on a 3mg/hr drip and admitted to the ICU. Patient ultimately was diagnosed with sick sinus syndrome and sustained a VT arrest in hospital.