EMory Files
Case #5: Massive PE
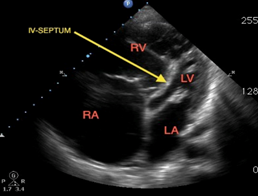
Hx: 40 yo F hx of Lupus presents with CP SOB
PE: VS: BP 90/50, HR 125, RR 30, O2 88%, afebrile. Awake and alert, mild distress improved with nonrebreather.
Case Discussion Massive PE:
***Case Discussion Wissam Jaber, Dir. PE Response Team***
https://www.dropbox.com/s/9xv0iqg5f4p9a0e/PE%20Jaber%20Interview.mp3
Teaching Point #1: Negative D-Dimer can exclude the diagnosis of PE in Wells low and moderate risk patients
Teaching Point #2: Massive PE=hypotension, Submassive=signs of heart strain (Echo, trop, BNP, or EKG changes)
Teaching Point #3: If your patient’s presentation isn’t even in the realm of PE, don’t start down the path.
Clinically Focused Review Article: Critical Issues in the Evaluation and Management of Adult Patients Presenting to the Emergency Department with Suspected Pulmonary Embolism. ACEP Clinical Policy. Fesmire et al. Annals of Emergency Medicine, June 2011. 6 questions answered:
1) Objective criteria versus gestalt? Objective criteria such as Wells Score, Modified Geneva Score, and Kline Rule produce similar accuracy to clinical gestalt when trying to assess a patient’s pre-test probability of PE. No rule is better than another and problems with inter-rater reliability plague both strategies (In other words, providers don’t always agree or consistently use the decision tools the same). Careful interns…experience affects gestalt!
2) What’s the role of PERC? PERC score can be used to rule out PE in Wells low risk patients. When applied to low risk patients, a negative PERC score makes the likelihood of a PE <2%. You are done!
3) What’s the role of D-Dimer? A negative D-Dimer can rule out PE in Wells low and moderate risk patients. At Grady, the threshold is <350. There is research suggesting doubling the threshold in low risk patients is safe, although it may miss clinically insignificant subsegmental PE’s.
4) What’s the role of CT PE? A negative CT PE protocol rules out the disease in low or moderate risk patients, but a negative CT PE may not be enough in high risk patients. D-dimer can actually be helpful in this situation where you are convinced a patient has a PE but the CT is negative. If the D-dimer is negative in this scenario, a PE is ruled out. If the D-dimer is +, you may have to push for a VQ or traditional pulmonary angiography, even if the CT PE is negative. You could also consider getting ultrasounds of LE in this scenario. If the dopplers are negative and the CT PE is negative, the likelihood of a PE is < 2% regardless of their pretest probability (i.e. Wells Score).
5) What’s the role of venous imaging? A + DVT US in patient presenting with symptoms consistent with PE establishes the diagnosis. In other words, if a patient has a contraindication to CT, a + DVT US in a patient with symptoms of PE establishes the diagnosis of PE. This is why we start with US in pregnant patients. You can also use US to rule out the diagnosis of PE in high risk patients that have a negative CT PE protocol. See question 4.
6) When do you give TPA? Hemodynamically unstable patients with PE. Consider it in patients with signs of R heart strain on echo or EKG (See embedded).
Case Resolution: Patient was diagnosed with massive PE. She had signs of R heart strain on EKG and bedside ultrasound. She had a troponin of 0.4. She was taken to the IR suite for catheter directed TPA. She improved clinically and was discharged on Coumadin.