Contributed by Jimmy Shah, Sanjana Rao, and Laura Galarza
FOOD ALLERGY 101
Did you know that over 15 million Americans suffer from food allergies today? Consider this. Every 3 minutes, a food allergy reaction sends someone to the ER. Given these severe, potentially life-threatening medical conditions that have no known cure, we think studying the origins of food allergies can have significant clinical implications. So what exactly is a food allergy?
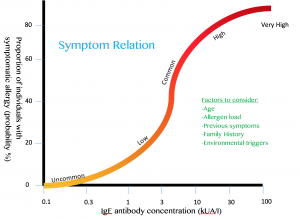
Food allergies manifest as adverse immune system reactions to harmless food substances. Once the allergen enters the body, it will be recognized by and bind to serum immunoglobulin E (IgE) – antibodies found in the lungs, skin, and mucosal membranes. IgE is attached by FcɛRI surface receptors on mast cells, an immune cell that helps the body create inflammatory responses. Interestingly, studies have shown that the high-affinity IgE-FcɛRI receptor binding is involved in responding to not only allergen exposure, but also parasite invasion.
After the binding occurs, the allergen will cause antibody cross-linking on the mast cell surface and lead to something called mast cell degranulation, which means the mast cell will release its internal pro-inflammatory molecules, like histamines, leukotrienes, and prostaglandins, into the bloodstream. This will cause the onset of the allergy symptoms many of us may know well (especially in the pollen-rich spring) – sneezing, itching, coughing, hives, GI discomfort, etc. The most severe of these is anaphylaxis, a rapid and potentially life-threatening body state where blood pressure is lowered and emergency symptoms arise as a result. This brings us to our central question: why would evolution naturally select for us to be allergic to food that sustains us? The anomaly of food allergies and their past, present, and future benefits remain largely poorly-defined. However, research shows us that IgE antibody recognition of the allergen and shared defense mechanisms play a significant role in evolving allergic responses over time.
EVOLUTION IN FOOD ALLERGY
Although not fully understood, allergic responses are thought to have evolved from an immune defense mechanism against parasite invasion and other harmful toxin colonization. For years, scientists saw allergies as genetic accidents where aberrant IgE antibody production was just a mishap. But given the conservative nature of evolution, the IgE antibody class couldn’t have just arisen to be destructive only in the case of genetic disorders. Even if they did, evolution wouldn’t keep them around if they were solely harmful. In 1991, Margie Profet created the toxin hypothesis – the idea that responding to toxins and allergic reactions occur in very similar ways, that allergies are inherently toxic or affiliated with toxic substances, and that allergic responses mostly involve symptoms by which toxins are expelled (sneezing, vomiting, coughing, etc.) Last month, scientists at Stanford published evidence supporting the sustained positive evolutionary pressure to keep these IgE antibodies around. First, they found that in normal mice, previous exposure to venom allowed for greater survivability following a lethal venom injection, as compared to mice who were only treated with control solution. Then, they tested the role of the allergic pathway. Specifically, they studied three different types of mice responding to bee venom injections – mice without IgE, mice without IgE receptors on mast cells, and mice without mast cells at all. Unlike the normal mice, the three mutants did not benefit from previous venom exposure, since they did not have the key immunological players coordinating allergic response (Tsai, 2015). Although allergies have become less threatening in our daily lives, this allergic-type, IgE-associated immune response provides support for the idea that allergic responses are closely linked to the ways in which our bodies fight off toxins, long ago and today.
In another study published in October 2015, researchers at the London School of Hygiene & Tropical Medicine hypothesized that there must be some molecular similarity between parasites and allergen proteins, as the same branch of the immune system is found to kick in in both circumstances. After extensive data analysis, the team found that 2,445 known parasite proteins were structurally and sequentially (think base pairs A, C, T, G) similar to those found in the portion of the allergen that is prone to immune system attack. Further, measuring human cell immune response to a protein from a parasitic worm that was similar to a protein from a prevalent pollen allergen family revealed that blood serum reacted against both worm infection and the allergen via the same antibody mechanism (Tyagi, 2015).
SIGNIFICANCE
Overall, the precise origin of food allergies has yet to be defined. However, we can infer that thousands of years ago, our ancestors may have consumed foods that contained harmful proteins or mimicked harmful substances, so allergies may have very well evolved to protect us. For example, someone could have ingested a raw plant that looked like a poisonous plant in the same family, so his body was on high alert. The IgE response naturally kicked in and perhaps was sustained throughout several generations as a heritable characteristic because it gave certain individuals an advantage over others in surviving and reproducing. As a result, those advantaged individuals likely passed on these beneficial traits, so eventually the proportion of individuals with these advantageous characteristics increased because those who didn’t, would lesser survivability.
This beneficial defense mechanism is not a novel idea – if unwanted substances enter the body, whether it just appears to be harmful or actually is, the organism’s ability to survive is potentially at stake. Thus, evolution would select for mechanisms by which these substances can be fought internally and expelled from the body. It therefore makes perfect sense that evolution would select for allergic responses as a means to protect one against destructive parasites and toxins.
Ultimately, food allergies account for $25 billion dollars in health costs each year, and cause 30,000 cases of anaphylaxis, 2,000 hospitalizations, and approximately 150 deaths annually. This significant burden on our population’s health warrants study of how allergic responses occur and the reasoning behind why they do. In doing so, perhaps we can find a cure! But for now, keep in mind that food allergies aren’t necessarily all bad and that they might actually be shielding you from something far worse.
FOR FURTHER READING…
Brandtzaeg, Per. 2010. Food Allergy: Separating the Science from the Mythology. Nature Reviews Gastroenterology & Hepatology 7, no. 7: 380–400.
Fitzsimmons, Colin Matthew, Franco Harald Fakone, and David William Dunne. 2014. Helminth Allergens, Parasite-Specific IgE, and Its Protective Role in Human Immunity. Frontiers in Immunology 5: 61.
Gross, Michael. 2015. Why did evolution give us allergies? Current Biology, no. 2: 53-55.
Liu, Andrew H. 2015. Revisiting the Hygiene Hypothesis for Allergy and Asthma. Journal of Allergy and Clinical ImmMatricardi, P. M. 2014. Molecular Evolution of the Allergy. Allergologie 37, no. 10: 423–24.
Machado, D. C., Horton, D., Harrop, R., Peachell, P. T. and Helm, B. A. (1996), Potential allergens stimulate the release of mediators of the allergic response from cells of mast cell lineage in the absence of sensitization with antigen-specific IgE. Eur. J. Immunol., 26: 2972–2980. doi: 10.1002/eji.1830261224
Platts-Mills, Thomas A. E. 2012. Allergy in Evolution. New Trends in Allergy and Atopic Eczema, edited by J. Ring, U. Darsow, and H. Behrendt, 96:1–6.
Ratnaparkhe, Milind B., Tae-Ho Lee, Xu Tan, Xiyin Wang, Jingping Li, Changsoo Kim, Lisa K. Rainville, et al. 2014. Comparative and Evolutionary Analysis of Major Peanut Allergen Gene Families. Genome Biology and Evolution 6, no. 9: 2468–88.
Sicherer, Scott H., and Hugh A. Sampson. 2009. Food Allergy: Recent Advances in Pathophysiology and Treatment. Annual Review of Medicine 60, no. 1 (2009): 261–77.
Tsai, Mindy, Phillip Starkl, Thomas Marichal. 2015. Testing the “toxin hypothesis of allergy: mast cells, IgE, and innate and acquired immune responses to venoms. Elsevier. Vol. 36: 80-87.
Tyagi, Nidhi, Edward Franell, Colin Fitzsimmons, Stephanie Ryan. Comparisons of Allergic and Metazoan Parasite Proteins: Allergy of the Price of Immunity. PLOS Computational Biology.
Wang, Jing, Litao Yang, Xiaoxiang Zhao, Jing Li, and Dabing Zhang. 2014. Characterization and Phylogenetic Analysis of Allergenic Tryp_alpha_amyl Protein Family in Plants Journal of Agricultural and Food Chemistry 62, no. 1: 270–78.
Zusi, Karen. 2015. An Evolutionary Basis for Allergies. The Scientist. http://www.the-scientist.com