Apr 17
Weekly Report – Baseball to the Eye

Apr 15
Image of the Week – Hepatic Abscess
The Image of the Week comes to us from Dr Layne Madden who used ultrasound to evaluate a patient who presented with fatigue, anorexia, and fever associated with epigastric pain on exam. Can you interpret the image below?
Thanks for all of your great images this week!
Happy Scanning!
===============================
Sierra Beck MD
Assistant Professor
Department of Emergency Medicine
Emory University SOM
Apr 12
Lit of the Week – Necrotizing Fasciitis
Clinical question / background:
- The goal of this study was to develop a diagnostic scoring system to distinguish necrotizing fasciitis from other soft tissue infections based on common laboratory evaluation.
Design:
- Retrospective observational study. Chart review of all patients diagnosed with necrotizing fasciitis (NF). Chart review of patients with cellulitis used as control.
- Initially developed rule with developmental cohort (n=314) and then validated with validation cohort (n=147).
- Inclusion criteria:
- Patients diagnosed with NF by chart review
- Control group of “severe soft tissue infections” identified by chart review of patients with documentation of soft tissue infection needing parenteral antibiotics for >48 hrs or abscess needing surgical debridement.
- Exclusion criteria:
- Minor soft tissue infection: length of stay less than 48 hours, oral antibiotics.
Outcome:
- Diagnosis of necrotizing fasciitis with scoring system as below (Based on developmental cohort)
- LRINEC scoring system:
- CRP (mg/L) ≥150: 4 points
- WBC count (×103/mm3)
- <15: 0 points
- 15–25: 1 point
- >25: 2 points
- Hemoglobin (g/dL)
- >13.5: 0 points
- 11–13.5: 1 point
- <11: 2 points
- Sodium (mmol/L) <135: 2 points
- Creatinine (umol/L) >141: 2 points
- Glucose (mmol/L) >10: 1 point
- Grouping by scoring
- Low Risk: score 5
- Moderate Risk: score 6-7
- High Risk: score >8
Results:
- LRINEC score >8 is strongly predictive of necrotizing fasciitis PPV 93%
- 89% of patients diagnosed with NF LRINEC score >6
- There were diagnoses of NF with LRINEC score of 0
Take-home:
- LRINEC score can raise suspicion of necrotizing fasciitis, however is not a “rule out”
- Does not replace clinical judgement
Weaknesses / Critiques
- Not prospectively validated.
Apr 11
FOAM of the Week – Pulmonary Hypertension, Hemoptysis, Pediatric Respiratory Disorders, The Transgender Patient

- Great overview of work up and treatment of Pulmonary Hypertension:
http://www.emdocs.net/the-crashing-pulmonary-hypertension-patient/
- A couple good posts on management of massive hemoptysis:
- In depth review of bronchiolitis from EMRAP:
- Or, shorter overview post (with great ddx of resp disorders in children at this bottom!):
http://dontforgetthebubbles.com/bronchiolitis/
- Great recent podcast on treating the transgender patient from EMRAP:
https://www.emrap.org/episode/springforward/transgender
Apr 02
Weekly Report – Tick Exposure
This week’s Weekly Report comes from Dr. Maryam Arshad:

A 37 year old male presents with flu like symptoms. He has a subjective fever, body aches, cough, and congestion. He also notes a recent tick bite one week ago and removed the tick by himself. He has no rash.
Clinical question:
Should this patient have Lyme titers drawn and should he be treated with antibiotics?
Lyme disease can be classified into three stages: ‘early’ or ‘localized’, ‘early disseminated’, or ‘late’. The early or localized stage typically occurs a few days to one month after the tick bite and is characterized by an erythema migrans rash. There may be some nonspecific complaints such as malaise, fever, and myalgias. Early disseminated stage occurs weeks to months after the tick bite. Patients may manifest symptoms that are cardiac (AV block), neurologic (meningitis or facial nerve palsy), or musculoskeletal (severe monoarticular arthritis). Late stage lyme disease occurs months to years after the initial tick bite and is most often associated with arthritis or neurologic disease.
Diagnosis of early or localized stage Lyme disease can be made clinically in patients with potential tick exposure who have an erythema migrans rash. In such patients, titers are likely to be negative as it takes several weeks to form an antibody response. Patients with erythema migrans should be empirically treated with oral doxycycline 100 mg BID for 10-21 days. Alternative regimens include amoxicillin 500 mg TID or cefuroxime axetil 500 mg BID. Patients with cardiac or neurologic manifestations may require IV therapy.
The CDC recommends that serologic testing should be performed on patients who have symptoms of early disseminated or late Lyme disease AND that meet the following criteria: a recent history of having resided in or traveled to an area endemic for Lyme disease and a risk factor for exposure to ticks. When serologic testing is indicated, a two-tier system is recommended: ELISA testing followed by a Western blot. It is possible for patients who were infected with Lyme to test negative if they received antibiotics early. Also, if testing is performed early, results may be falsely negative as the antibody response typically takes a few weeks to develop, so if clinical suspicion is high convalescent serum testing is recommended.
Routine use of antibiotic prophylaxis or serologic testing after a tick bite in a patient who is asymptomatic is not recommended. However, if all of the following criteria are met, a single dose of 200 mg doxycycline may be offered for prophylaxis against Lyme: 1) the tick can be identified as Ixodes scapularis with an estimated time of attachment >36 hours based on degree on engorgement or exposure time; 2) prophylaxis can be administered within 72 hours of tick removal; 3) local rates of infection of these ticks with Borrelia burgdorferi is >20%; 4) doxycycline is not contraindicated.
For more information: http://www.cdc.gov/lyme/healthcare/index.html
References:
- Wormser et al. The Clinical Assessment, Treatment, and Prevention of Lyme Disease, Human Granulocytic Anaplasmosis, and Babesiosis: Clinical Practice Guidelines by the Infectious Disease Society of America. Clin Infect Dis. (2006) 43 (9): 1089-1134.
- Centers for Disease Control and Prevention (CDC). Tickborne Diseases of the United States: A Reference Manual for Health Care Providers, Third Edition (2015).
- Centers for Disease Control and Prevention (CDC). Recommendations for test performance and interpretation from the Second National Conference on Serologic Diagnosis of Lyme Disease. MMWR Morb Mortal Wkly Rep 1995; 44:590.
- Shapiro ED, Gerber MA, Holabird NB, et al. A controlled trial of antimicrobial prophylaxis for Lyme disease after deer-tick bites. N Engl J Med 1992; 327:1769.
- Steere AC. Diagnosis and treatment of Lyme arthritis. Med Clin North Am 1997; 81:179.
- Nadelman et al. Prophylaxis with single-dose doxycycline for the prevention of Lyme disease after an Ixodes scapularis tick bite. N Engl J Med. 2001 Jul 12;345(2):79-84.
Apr 01
Image of the Week – Superficial and Deep Peroneal Nerve Block
The Image of the Week comes to us from Drs. Karen Bowers and Mene Demestihas who used ultrasound to assist with anesthesia to a complex laceration involving the dorsum of the foot and first web space. They performed two nerve blocks, one of which is shown below. How would you anesthetize a wound like this?
Thanks for all of your great images this week!
Happy Scanning!
===============================
Sierra Beck MD
Assistant Professor
Department of Emergency Medicine
Emory University SOM
Mar 29
Lit of the Week: Prehospital hypoxia in TBI
Clinical question / background:
- The goals of this study were to determine the incidence and duration of hypotension (SBP <90) and hypoxia (SpO2<92%) in the prehospital setting in patients with potentially survivable brain injuries, and to prospectively examine the association of these secondary insults with mortality and disability.
Definitions:
- Hypotension: SBP< 90mmHg
- Hypoxia: SpO2 < 92%
- Disability rating scale: 0-30 scale with >20 very severe.
- Abbreviated injury scale: score of 0-6 for scale of injury to specific body area. 0 being mild and 6 being maximal injury.
Design:
- Prospective cohort study
- 150 trauma patients at 4 different level 1 trauma centers, identified as having suspected head injury by flight medic/nurse
- Inclusion criteria:
- Diagnosis of acute traumatic brain injury confirmed by CT, operative findings or autopsy
- Head Abbreviated Injury Scale of 3 or greater or GCS 12 or less within first 24 hours of admission. *not influenced by alcohol, sedatives, or muscle relaxants
- Exclusion criteria:
- No abnormal intracranial findings on CT scan
- Non-survivable injury (AIS score of 6 for any body region)
- Death less than 12 hours after injury
Outcome:
- Primary outcome: Mortality.
- Secondary outcomes
- Hospital LOS
- Disability rating scale (Range 0-29) at discharge
Results:
- Mortality:
- Overall: 23.3%
- With prehospital secondary insults: 28%
- Without prehospital secondary insult: 20%
- LOS (days)
- Without insult: 20 days
- With insult: 27 days (p03)
- Disability rating scale at discharge
- Without insult: 10
- With insult: 14 (p02)
Take-home:
- The acute care of patients with traumatic brain injury begins in the prehospital setting. Both hypoxia and hypotension exacerbate traumatic brain injury and lead to worse outcomes. The authors note that as secondary insult, isolated hypoxia is associated with increased mortality while isolated hypotension is not. In both the prehospital setting and while in the emergency department, care should me taken to optimize oxygenation/ventilation and maintain blood pressure.
- The independent variables that were identified as affecting mortality were: hypoxia, older age, lower GCS score, Marshall score, head AIS score, and multiple traumatic injuries significantly affected mortality.
- Multivariate analysis accounting for the above independent variables showed that hypoxia was an independent predictor of mortality (OR 2.66, p 0.05). Age >65 years and GCS score <8 were also significant predictors of mortality in multivariate analysis, but hypotension was not.
Weaknesses / Critiques
- This study excluded those who died within 12hours after injury, perhaps those with the most lethal injuries. Interestingly, most previous data found that hypotension and not hypoxia (the reverse findings of this paper) was linked with increased mortality in TBI. The authors suggest that the exclusion of these high lethality injuries could explain for this discrepancy.
Mar 29
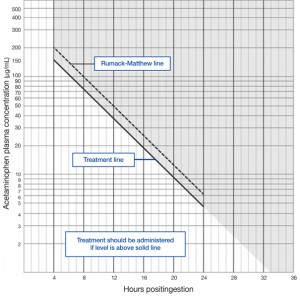
Lit of the Week — Acute Acetaminophen Toxicity and NAC
Lit of the Week – 3/29/16
Rumack BH, Peterson RC, Koch GG, Amara IA. Acetaminophen overdose. 662 cases with evaluation of oral acetylcysteine treatment. Arch Intern Med. 1981 Feb 23;141(3 Spec No):380-5. PubMed PMID: 7469629.
http://www.ncbi.nlm.nih.gov/pubmed/7469629
Clinical question / background:
- Does N-acetylcysteine prevent or moderate hepatotoxicity secondary to acute acetaminophen overdose?
Design:
- Nationwide, multiclinic open study
- Started in 1976 at the Rocky Mountain Poison Center, Denver
- 662 consecutive patients with acetaminophen overdose
- Inclusion: Age > 12 y/o, history of known or suspected acute ingestion of 7.5 g or more of acetaminophen within 24 hours of presentation, plasmal acetaminophen level in toxic range on the nomogram
- Exclusion: ingestion > 24h old
- Primary outcome: incidence of hypotoxicity secondary to acute acetaminophen ingestion
- Clinically significant hepatotoxicity defined as AST > 1000 IU/L
- Patients grouped based on time of ingestion to administration of NAC
- < 10 hours
- 10-16 hours
- 16-24 hours
- Secondary outcomes: mortality, safety of oral NAC
Intervention:
- NAC loading dose: 140 mg/kg PO x 1
- NAC maintenance dose: 70 mg/kg PO q4 for 17 additional doses
- Supportive measures, gastric lavage up front
Control:
- None
Results:
- Incidence of hepatotoxicity and time to treatment for patients with acetaminophen concentration in probable toxic range (line intersecting 200 mg/mL (1324 mmol/L) at 4 hours and 50 mg/mL (331 mmol/L) at 12 hours) were:
- 7% when treated within 10 hours of ingestion
- 29% when treated within 10 to 16 hours of ingestion
- 62% when treated within 16 to 24 hours of ingestion
- Statistically significant trend in reduction severity of toxicity with earlier onset of NAC treatment
- Alcohol congest as possible protective effect
Take-home:
- NAC is a safe and effective management option of acetaminophen overdose and its effects are more beneficial with early administration < 10 hours after overdose ingestion
Strengths:
- Large study
- Simple protocol with reproducible results in subsequent studies
- Mainstay of treatment for acetaminophen overdose remains NAC
Weaknesses / Critiques
- No control
- Unable to ascertain effects on chronic ingestion
- PO administration only
Follow-up / Real World Application
- Acute Acetaminophen Ingestion – remember that Rumack-Mathew Nomogram ONLY for acute ingestions
- VERY IMPORTANT to ascertain INGESTION TIME – use EARLIEST if patient took multiple ingestions over a period of hours
- Call Poison control center à 5-9000, ext 2; (404-616-9000 ext. 2)
- Ingestion < 4 hours
- AC if < 3 hours post-ingestion
- Send 4-hour APAP level and treat if necessary
- Ingestion 4-24 hours
- If APAP level available by 8 hours post-ingestion, can wait before starting NAC
- If APAP level will be available > 8 hour post-ingestion or patient presenting > 8hours post ingestion, START NAC and send APAP level to guide treatment
- Ingestion > 24 hours or unknown ingestion time
- Send APAP level, LFTs, Coags, ABG
- Give 1st dose of NAC
- If APAP level > 10, or elevated LFTs à continue NAC
- pH <7.3, PT > 100, Cr >3.3 or AMS, consider transplant eval
- If APAP level normal and LFTs wnl, stop NAC
- NAC Dosing
- PO – 72 hr protocol
- 140 mg/kg PO load
- 70 mg/kg PO q4hr x 17 additional doses
- IV – 21 hr protocol
- Load: 150 mg/kg in 100 mL D5W over 60 min
- Maintenance: 50 mg/gk in 250 mL D5W over 4 hrs
- Third dose: 100 mg/kg in 500 mL D5W over 16 hrs
- PO – 72 hr protocol
- Ingestion < 4 hours
Mar 25
Image of the Week – Intussusception
The image of the week this week comes to us from Drs. Brandi Gunn and Jeff Siegelman who used bedside ultrasound to evaluate an adult with nausea and abdominal pain. They obtained and correctly interpreted the image below. Can you make the diagnosis?
Thanks for all of your great images this week!
Happy Scanning!
===============================
Sierra Beck MD
Assistant Professor
Department of Emergency Medicine
Emory University SOM
Mar 22
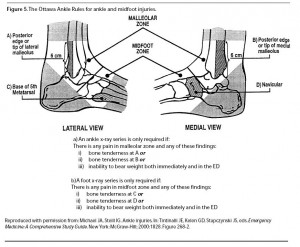
Lit of the Week — Ottawa Ankle and Foot Rules
Lit of the Week – 3/01/16
Clinical question / background:
- Can decision rules based on history and simple physical exam findings guide the use of radiography in acute ankle and foot injuries?
Design:
- Prospective study of 1032 patients with acute ankle injuries refining old ankle rules followed by validation in 453 patients
- 2 urban academic center emergency departments
- Inclusion: Adults (> 18 y/o) presenting after acute blunt ankle trauma
- Exclusion: Pregnant patients, children, injury > 10 days old, OSH transfers, patients returning for reassessment of same injury
- Patient evaluated by one of 21 study physicians according to pre-determined decision rules (details below)
- Primary outcome: detection of clinically significant fracture which is defined as fracture or avulsion > 3 cm
- Secondary outcomes: interobserver reliability
Intervention of Ankle and Foot Rules
- Ankle Rules – ankle x-ray indicated for following physical findings
- Bony tenderness along posterior edge or tip of distal 6 cm of lateral malleolus
- Bony tenderness along posterior edge or tip of distal 6 cm of medial malleolus
- Inability to bear weight on injured extremity both immediately after injury or in the emergency department (four steps)
- Limping counts as bearing weight
- Foot Rules – foot x-ray indicated for following physical findings
- Bony tenderness at the navicular (medial aspect of foot)
- Bony tenderness at the base of the 5th metatarsal
- Inability to bear weight on injured extremity both immediately after injury or in the emergency department (four steps)
- Limping counts as bearing weight
Results:
- Ankle Rules
- Sensitivity 100%, Specificity 39% in refinement cohort
- Sensitivity 100%, Specificity 49% in validation cohort
- Foot Rules
- Sensitivity 98%, Specificity 70% in refinement cohort
- Sensitivity 100%, Specificity 79% in validation cohort
Take-home:
- If ankle pain is present and there is tenderness over the posterior 6 cm or tip of the posterior or lateral malleolus, then an ankle-ray is indicated
- If midfoot pain is present and there is tenderness over the navicular or the base of the fifth metatarsal, then a foot-xray is present
- If there is ankle or midfoot pain and the patient is unable to take four steps both immediately and in the emergency department, then x-ray of the painful area is indicated
- In patients that fail to fulfill the above rules, radiography likely not indicated but defer to clinical judgment
Strengths:
- Well-designed, large study
- High kappa values indicating interobserver reliability
- e. multiple examining physicians likely to get similar exam results on patients and implement rules appropriately
- can reduce # of x-rays and speed up patient turnover in ER
Weaknesses / Critiques
- poor specificity in the ankle cohort, relatively weak specificity in foot cohort
- not useful for calcaneal injuries, distal foot injuries
- careful with patients who are intoxicated, uncooperative, have painful or distracting injuries, or diminished neurologic function in extremity that can limit usefulness of exam